Arthritis
Understanding Lifestyle Risk Factors and Modifiable Behaviors
Discover > Health Conditions > Arthritis
Arthritis encompasses a range of joint disorders characterized by inflammation and pain. While genetics and age are non-modifiable factors contributing to the onset and progression of conditions such as osteoarthritis and rheumatoid arthritis, certain lifestyle choices and behaviors have been identified as modifiable risk factors. These lifestyle elements provide an avenue for individuals to possibly prevent or mitigate the severity of arthritis symptoms through informed changes in daily habits.
Among the risk factors, smoking has been consistently linked with an increased risk of developing rheumatoid arthritis and exacerbating its symptoms. It's noted that smoking may not only initiate the inflammatory processes associated with arthritis but can also interfere with the effectiveness of treatments. Similarly, maintaining physical activity is beneficial in managing arthritis symptoms and mobility. A sedentary lifestyle, on the other hand, may contribute to the worsening of arthritis symptoms and overall joint health. It's also suggested that dietary choices play a role in the management of arthritis, with balanced, nutrient-dense diets offering potential benefits in reducing inflammation and maintaining healthy body weight.
These aspects highlight the importance of lifestyle management in the context of arthritis. Making informed choices in areas such as smoking cessation, engaging in joint-friendly exercise, and adhering to a nutritious diet can be pivotal in the management and outcome of arthritis, providing individuals with actionable steps to influence their health.
Fundamentals of Arthritis
Arthritis encompasses various conditions characterized primarily by joint pain and inflammation. It is important for individuals to understand the basic concepts of arthritis to better grasp its impact on health.
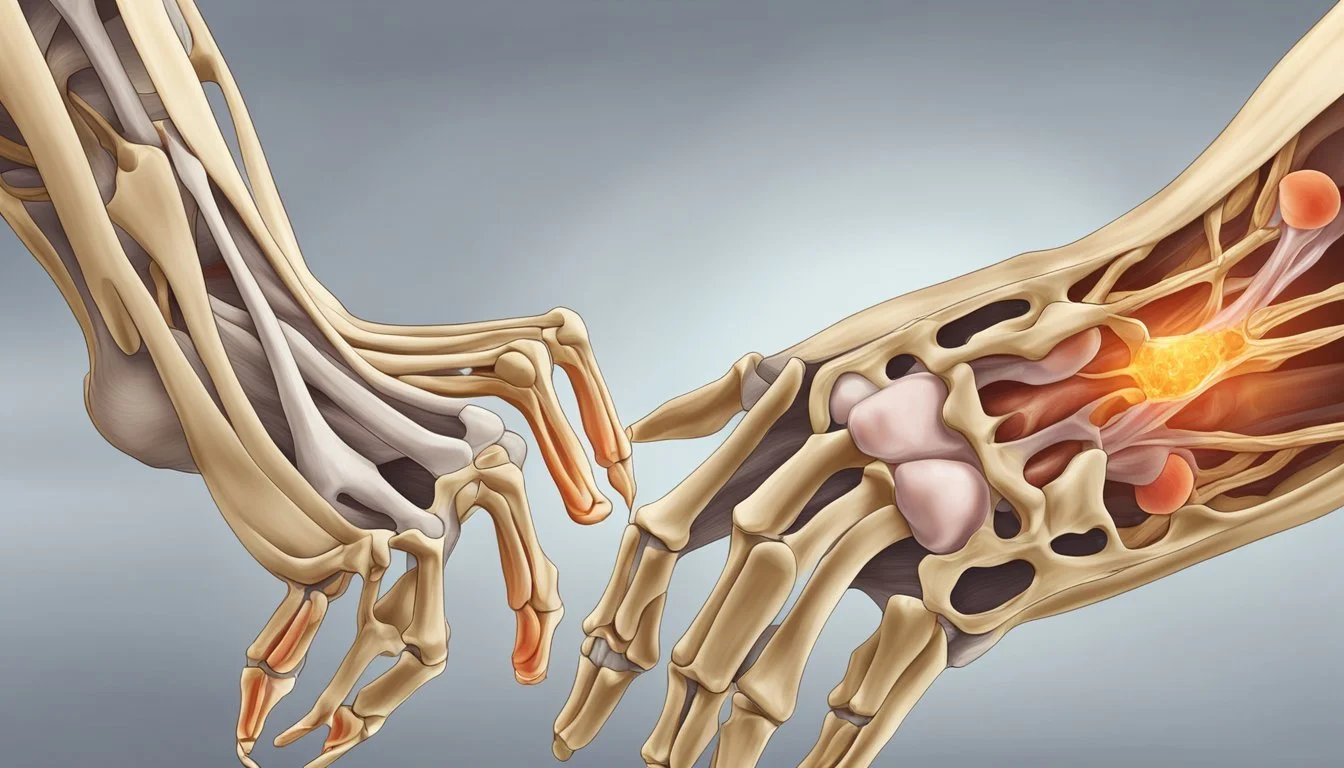
Defining Arthritis
Arthritis is a broad term used to describe conditions that affect the joints, tissues surrounding the joints, and other connective tissues so there are many types of arthritis that someone can suffer from. The most notable symptoms include joint pain and stiffness, which typically worsen with age.
Types of Arthritis
Osteoarthritis
Definition: The most common form of arthritis, where the protective cartilage that cushions the ends of the bones wears down over time.
Affected Joints: Typically affects the hands, knees, hips, and spine.
Symptoms: Pain, swelling, reduced range of motion, and stiffness in the affected joints.
Rheumatoid Arthritis
Definition: An autoimmune disease where the immune system mistakenly attacks the joints, causing inflammation.
Affected Joints: Often impacts the joints in the hands, wrists, and knees.
Symptoms: Tender, warm, swollen joints and stiffness that is usually worse in the mornings or after inactivity.
Both types of arthritis lead to chronic symptoms and can result in significant discomfort and disability if not managed effectively.
Genetic and Non-Modifiable Arthritis Risk Factors
Arthritis is influenced by a complex interplay of genetic and non-modifiable factors that elevate the risk factors of disease development. Understanding these elements is crucial for recognizing individuals at higher risk.
Age and Sex
Arthritis risk generally increases with age, as the wear and tear on joints accumulate over time. Moreover, sex is a significant determinant, with females being more predisposed to certain types, like rheumatoid arthritis (RA), owing to hormonal influences and other unknown factors tied to gender.
Genetic Predisposition
Genetics carry a notable influence on whether or not you are likely to develop arthritis. Specific genes related to the immune system's function can lead to a higher susceptibility. For example, the presence of the HLA-DR4 allele has been linked to an increased risk for RA.
Individuals with a family history of arthritis, particularly immediate family members, are at a higher risk. This suggests a heritable component, where genetics and family-shared environments may contribute significantly to disease risk. Autoimmune diseases in the family tree can further signify an elevated predisposition to arthritis.
Lifestyle choices significantly influence the risk and management of arthritis, particularly concerning obesity, diet, and substance use. Addressing these factors can help reduce the likelihood that one might develop arthritis or mitigate its severity.
Obesity and Physical Activity
Maintaining a healthy weight is crucial in reducing the pressure on joints and lowering the risk of developing osteoarthritis. Extra weight stresses weight-bearing joints like hips and knees. Physical activity not only helps in weight management but also improves joint flexibility and strength. It is recommended to engage in regular, moderate exercise to support joint health.
Diet and Nutrition
A balanced diet plays a role in managing arthritis risk. Anti-inflammatory foods, such as fruits, vegetables, and omega-3-rich fish, can support joint health. Conversely, a diet high in processed foods and sugars may increase inflammation, contributing to arthritis symptoms. Adequate nutrition supports maintaining a healthy weight, which is another modifiable risk factor for arthritis.
Smoking and Alcohol Consumption
Cigarette smoking has been identified as a modifiable risk factor, especially for rheumatoid arthritis. It can exacerbate the disease and lead to other health complications. Reducing or ceasing smoking can mitigate these risks. Moderate alcohol consumption may offer some protective benefits against certain types of arthritis, while excessive alcohol use can be detrimental and is considered a risk factor.
Medical Conditions and Other RISK Factors
Several medical conditions and lifestyle risk factors are linked to an increased risk of developing arthritis. This section explores how infections and immunity, past joint injuries, and one's occupation and activity level can influence the likelihood of arthritis development.
Infections and Immunity
Infectious agents, such as bacteria and viruses, can trigger joint inflammation and contribute to the development of certain types of arthritis. For example, bacteria like those that cause Lyme disease can lead to infectious arthritis if not treated promptly.
Immune System: Conditions that involve the immune system, such as lupus and rheumatoid arthritis (RA), occur when the immune system mistakenly attacks the body's own tissues, including joints. This immune response can lead to chronic inflammation and joint damage.
Previous Joint Injuries
Injuries to joints, whether from sports or accidental trauma, can increase the risk of developing arthritis in those joints later in life.
Joint Injury: A history of joint injury is a known risk factor, particularly if the injury was severe or if the joint was not properly rehabilitated.
Sports: Athletes, especially those in contact sports, may experience repetitive stress injuries which can compromise joint integrity and function.
Occupation and Activity Level
Certain occupations and activities that place repetitive stress on joints can contribute to the development of arthritis.
Occupation: Jobs involving kneeling, squatting, or lifting heavy weights can put excessive stress on weight bearing joints and lead to joint problems.
Repetitive Stress: Repetitive motion or overuse of particular joints in daily activities or through occupational tasks, such as repetitive knee bending, can result in pain and stiffness and potentially lead to arthritis over time.
Occupational factors and activity levels, along with medical history, play a critical role in determining an individual's risk for arthritis. By recognizing and addressing these factors, individuals may reduce their risk or manage the impact of arthritis on their lives.
Clinical Symptoms and Diagnosis
Arthritis diagnosis involves recognizing the characteristic symptoms and conducting medical assessments by healthcare professionals. Understanding the manifestations and the diagnostic steps is essential for patients seeking clarity about their condition.
Joint Pain and Other Symptoms
Patients typically report several clinical symptoms associated with arthritis. The symptoms may include, but are not limited to:
Pain: A hallmark symptom, often worsening after activity or towards the end of the day.
Stiffness: Notably distinct in the morning, lasting more than thirty minutes.
Swelling: Joints may swell due to inflammation or fluid and uric acid crystal accumulation.
Redness and Warmth: The affected area might appear redder and feel warm to the touch.
Tenderness: Joints may be sensitive to pressure or touch.
Decreased Range of Motion: Difficulty in movement or completing daily tasks may occur.
Patients with rheumatoid arthritis might experience periodic flares, with symptoms temporarily intensifying when there is too much uric acid present. In those with psoriatic arthritis, skin symptoms like psoriasis often precede joint issues.
Diagnostic Process
When a patient presents symptoms indicative of arthritis, the doctor will initiate a diagnostic evaluation comprising:
Medical History: A complete review to assess symptoms, their onset, and family history of arthritis.
Physical Examination: Examining the affected joints for swelling, redness, warmth, and mobility.
Laboratory Tests: Blood tests to look for inflammatory biomarkers or specific antibodies, like rheumatoid factor.
Imaging: X-rays, MRI, or ultrasound scans can reveal the extent of joint damage.
Early diagnosis of the types of arthritis and appropriate treatment are often crucial to managing symptoms effectively and preventing further joint damage.
Consequences and Complications
Arthritis can significantly detract from an individual’s quality of life, leading to a range of physical complications and mental health challenges. Recognizing these consequences is critical for managing the condition effectively.
Arthritis is primarily associated with joint damage, which can manifest as deformities and wear-and-tear damage to the cartilage. This deterioration often results in joint stiffness, especially in the morning, and can severely limit mobility.
As the severity of the condition increases, individuals may experience chronic arthritis pain and fatigue, making daily activities challenging. The inflammation that characterizes many forms of arthritis can also lead to systemic issues, such as fever in more acute cases.
If you develop rheumatoid arthritis symptoms you should seek your healthcare provider.
The persistent discomfort and reduced mobility associated with arthritis often contribute to mental health challenges. Individuals living with arthritis have an elevated risk of developing depression, stemming from chronic pain and decreased participation in activities they once enjoyed.
The continuous battle against fatigue and the frustration over a loss of independence can exacerbate these mental health struggles, necessitating support and sometimes professional counseling.
Treatment Approaches
Effective arthritis management involves a comprehensive treatment plan that addresses medications, lifestyle modifications, and, if necessary, certain types of arthritis may require surgical intervention. These strategies are aimed at reducing pain and inflammation, maintaining a healthy weight, and preserving joint function.
Arthritis treatment typically begins with medications from healthcare providers. Nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids are commonly prescribed to reduce inflammation and alleviate pain. Methotrexate is often the first-line disease-modifying antirheumatic drug (DMARD) for rheumatoid arthritis, and it can induce remission in some cases. Biologic response modifiers, another class of DMARDs, are used when conventional treatments are ineffective.
NSAIDs: Ibuprofen, naproxen
Corticosteroids: Prednisone
DMARDs: Methotrexate, leflunomide
Biologics: Etanercept, infliximab
Lifestyle changes play a critical role in managing arthritis symptoms and improving quality of life. Patients are encouraged to maintain a healthy weight to reduce stress on the joints. Incorporating physical activity into one's routine enhances muscle strength and joint flexibility, which can alleviate pain.
Healthy Weight Management:
Balanced diet
Portion control
loss of excess weight
Physical Activity:
Low-impact exercises: Swimming, walking
Stretching and strength training
Surgical Options
Surgery may be considered by your healthcare provider when severe arthritis has damaged joints, and other treatments have not provided adequate relief. Joint replacement surgery, such as hip or knee replacements, restores function and reduces pain. Arthroscopic procedures can repair joint damage minimally invasively.
Surgical Treatments:
Joint replacement: Hip, knee
Arthroscopy: Joint repair
Emerging Research and Future Perspectives
Recent studies in rheumatoid arthritis (RA) have brought to light the role of modifiable lifestyle factors and genetic predispositions in disease onset and progression. With a focus on prevention and early detection, these areas represent avenues for potentially reducing RA risk through targeted interventions.
Innovative Treatments
Investigators are exploring treatment options for specific types of arthritis that specifically modulate the immune system to prevent the development of autoimmunity in at-risk individuals.
Advanced understanding of cytokine actions and their impact on RA has led to therapies aimed at intercepting cytokine signaling pathways. Additionally, biologic agents that target specific components of the immune response, for instance, B-cells which produce disease-related antibodies, are becoming increasingly refined.
Genetic Research
Genetic research has uncovered numerous loci that contribute to the susceptibility to autoimmune diseases, including RA. Mapping the human genome permits the identification of genetic markers that can be used to predict RA risk.
For instance, the presence of certain genes may correspond with autoantibody production, a precursor to overt disease. Researchers are also examining how genetic risk factors interact with potential pathogens that may trigger immune system attacks or exacerbate the autoimmune response in RA.