Dermatitis
Symptoms, Causes, and Home Remedies
Discover > Health Conditions > Dermatitis: Symptoms, Causes, Home Remedies
Dermatitis, a common skin condition, affects individuals of all ages, often causing discomfort and impacting their quality of life. It manifests as inflammation of the skin, leading to symptoms such as redness, itching, and sometimes blistering or cracking. While there are various types of dermatitis, the most prevalent forms include atopic dermatitis (eczema), contact dermatitis, and seborrheic dermatitis.
Understanding the causes and triggers of dermatitis is essential for effective management of the condition. Generally, dermatitis results from a combination of genetic and environmental factors. Some people may have a genetic predisposition that weakens the skin's barrier function, making them more susceptible to environmental irritants, allergens, and infections. Contact with certain substances, such as chemicals, plants, or cosmetics, may also provoke an immune response that causes skin inflammation.
Although there is no cure for dermatitis, numerous home remedies can provide relief from its symptoms and improve one's skin health. These treatments may include the use of moisturizers, cold compresses, and over-the-counter anti-inflammatory creams. Additionally, making lifestyle changes such as avoiding known irritants, managing stress, and maintaining a balanced diet can go a long way in managing and reducing the occurrence of dermatitis flare-ups.
Understanding Dermatitis
Dermatitis is a general term used to describe a variety of skin conditions characterized by inflammation of the skin. It is commonly manifested as a rash, which can be itchy, red, and sometimes painful. Dermatitis has several types, including atopic dermatitis, contact dermatitis, seborrheic dermatitis, and neurodermatitis. In this section, we will discuss the various types of dermatitis and the factors that contribute to their development.
Atopic dermatitis, also known as eczema, is a chronic skin condition that commonly affects children but can also occur in adults. It is characterized by itchy, dry, and inflamed patches of skin. The exact cause of atopic dermatitis is not completely understood, but it is believed to be a combination of genetic predisposition and environmental factors. Some common triggers include irritants, allergens, low humidity, and stress.
Contact dermatitis occurs as an allergic or irritant reaction to substances that come into contact with the skin. This type can be divided into two categories:
Allergic contact dermatitis - caused by an immune reaction to allergens, such as metals, chemicals, and plants.
Irritant contact dermatitis - occurs due to direct damage to the skin from irritants like detergents, acids, or solvents.
Seborrheic dermatitis affects areas of the skin that are rich in oil-producing glands, such as the scalp, face, and upper chest. It is characterized by redness, scaling, and flaking of the skin. The exact cause of seborrheic dermatitis is not well understood, but it is thought to involve an overgrowth of the yeast Malassezia on the skin and an abnormal immune response.
Neurodermatitis is a skin condition resulting from repetitive scratching or rubbing of the skin, typically caused by stress or anxiety. This constant irritation leads to a vicious cycle of itching and scratching, resulting in thickened and leathery skin.
In conclusion, dermatitis has various forms and causes, making it essential to understand the specific type and its triggers to manage the condition effectively. By being aware of the possible factors that contribute to the development of each type, individuals can take the necessary steps to prevent flare-ups and maintain healthy skin.
Symptoms and Recognition
Physical Manifestations
Dermatitis is characterized by various symptoms and signs that result in discomfort and skin irritation. The most common symptoms include:
Dry skin: The affected area becomes rough, tight, and even cracked.
Itchiness: An intense, persistent itch leads to the urge to scratch the affected area.
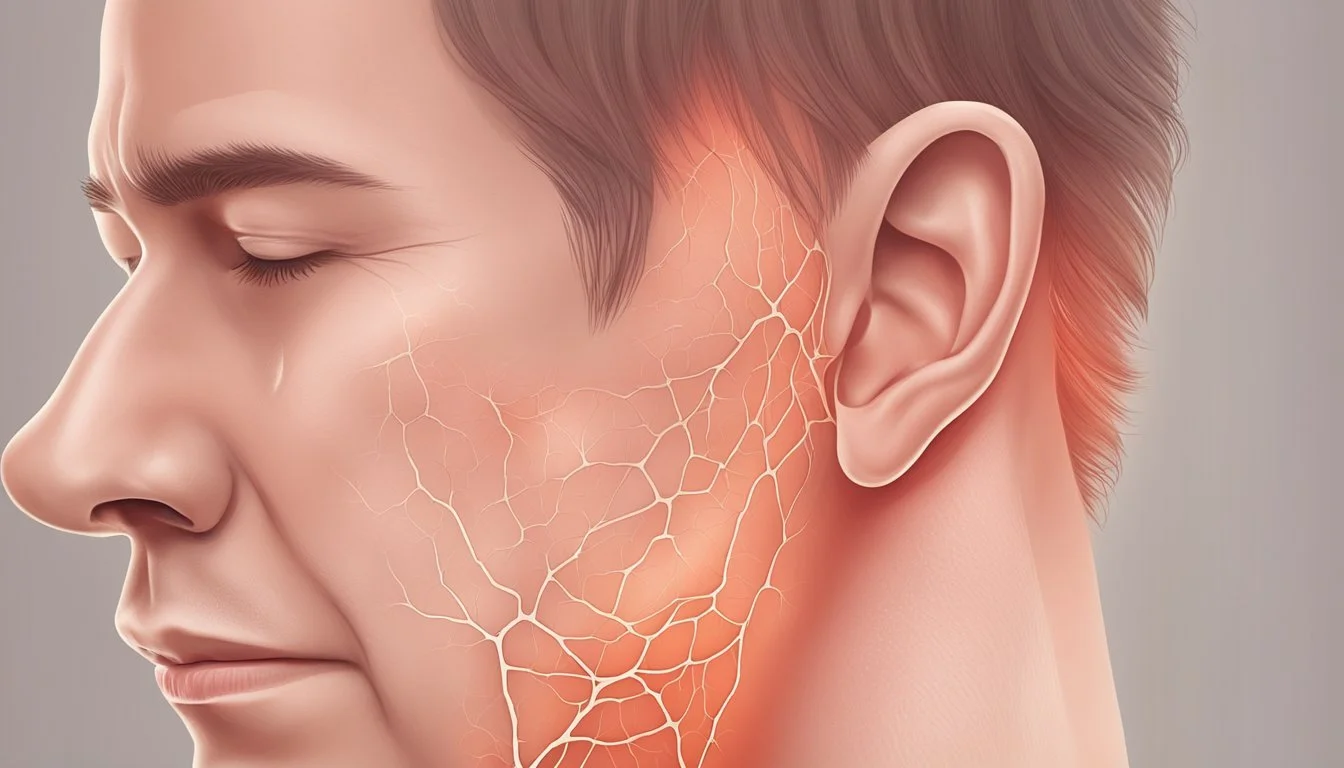
Inflammation: The skin becomes red, swollen, and warm to the touch.
Red rash: A visible red rash with uneven borders may appear on the affected area.
Blisters and crust: Small fluid-filled blisters may develop, which can burst, and then form a crust or scab.
Pattern and Location
The pattern and location of dermatitis can vary depending on the type and severity of the condition. Common locations where dermatitis may manifest include:
Face: Dermatitis often appears on the cheeks, forehead, and around the nose.
Neck: The skin on the front, sides, or back of the neck can be affected.
Hands: The palms, backs of hands, and skin between the fingers can become inflamed and irritated.
Feet: The condition can affect the tops and soles of feet, as well as the skin between the toes.
Knees: Dermatitis may appear on the front or back of knees or around the knee joint.
Scalp and head: The condition can cause skin irritation, dryness, and flaking on the scalp and behind the ears.
Legs: Dermatitis can cause red rashes and patches on the shins or thigh areas.
It is essential to recognize the symptoms and patterns of dermatitis to seek appropriate treatment and manage the condition effectively.
Causes and Triggers of Dermatitis
There are multiple factors that contribute to the development of dermatitis, from genetic predisposition to environmental exposures. This section outlines the primary causes and triggers of the condition, organized into four major categories.
Allergens and Irritants
A common cause of dermatitis is the exposure to allergens or irritants, which can provoke an inflammatory skin reaction. Examples include:
Soaps and detergents: Harsh cleaning agents can strip away the skin's protective oils, resulting in irritation or an allergic reaction.
Cosmetics and fragrances: Certain chemicals found in personal care products may trigger dermatitis in sensitive individuals.
Metals and materials: Items like jewelry, clothing, or even elastic bands can be sources of skin contact allergens, such as nickel.
Plants and insects: Poison ivy, poison oak, and insect stings or bites sometimes lead to a localized dermatitis reaction.
Genetics and Immunity
Individuals with a history of atopic conditions, such as asthma or hay fever, are more likely to develop dermatitis. Research suggests that an inherited predisposition to these conditions can make a person more susceptible to dermatitis by affecting their immune system. In addition, those with compromised immune function, such as individuals with HIV, may experience more severe symptoms or frequent flare-ups.
Environmental and Personal Factors
Several personal or environmental circumstances may influence the development or severity of dermatitis:
Stress: High levels of stress can weaken the immune system, making an individual more vulnerable to dermatitis flare-ups.
Age: Certain types of dermatitis, like seborrheic and atopic dermatitis, are more common in infants and children, whereas others may develop later in life.
Sweat and bacteria: A moist environment can encourage the growth of fungus or bacteria, which can aggravate dermatitis or lead to secondary infections.
Food allergies: Some people may experience dermatitis when consuming specific foods to which they have allergies or intolerances.
Physical pressure: Rubbing or scratching can induce symptoms of dermatitis, which is commonly experienced by those suffering from dermatitis herpetiformis.
Medications: Certain medications, such as antibiotics, can sometimes trigger a dermatitis flare.
Specific to Types of Dermatitis
Each type of dermatitis has its unique causes and triggers:
Atopic dermatitis: An overactive immune system and malfunctioning skin barrier are the primary causes, with triggers such as allergens, irritants, infections, and emotional stress.
Contact dermatitis: Allergic contact dermatitis arises from an immune response to specific substances. In contrast, irritant contact dermatitis results from direct damage to the skin by chemicals or physical agents.
Seborrheic dermatitis: Although its exact cause is unknown, it appears to be influenced by factors like genetics, stress, and the presence of a specific yeast called Malassezia.
Dyshidrotic eczema: The exact cause remains unknown; however, it may be related to seasonal allergies, stress, or exposure to certain metals or chemicals.
Populations Mostly Affected
Dermatitis, a common skin condition, affects various age groups, but certain forms of it prevail more among specific populations. In this section, we will discuss which age groups are more susceptible to different types of dermatitis.
Atopic Dermatitis: This form primarily affects infants and young children. According to studies, nearly 90% of cases appear before the age of 5, and over 60% manifest within the first year of life. Although it may start during infancy, atopic dermatitis often persists into adulthood for some individuals.
Contact Dermatitis: Both adults and children are prone to developing contact dermatitis, which is caused by skin contact with allergens or irritants. However, the prevalence of this type of dermatitis may be slightly higher in adults, who are more likely to encounter such substances in their daily lives, e.g., at their workplace or through exposure to personal care products.
Seborrheic Dermatitis: This form of dermatitis typically affects two distinct age groups:
Infants: Seborrheic dermatitis can occur during the first few months after birth, commonly known as "cradle cap." It usually resolves within the first year.
Adults: The prevalence of seborrheic dermatitis peaks again in middle-aged adults, particularly among those aged 30-60 years.
Diaper Dermatitis: As the name suggests, this form of dermatitis affects babies and infants wearing diapers. It occurs due to the moist and warm environment created by diapers, combined with irritants from urine and feces. Proper hygiene and frequent diaper changes can help prevent diaper dermatitis.
In conclusion, various types of dermatitis affect different age groups, with atopic dermatitis being more common among infants and children, while contact dermatitis and seborrheic dermatitis are more prevalent in adults. Diaper dermatitis affects those in early infancy.
Diagnosing Dermatitis
In order to diagnose dermatitis effectively, a healthcare professional will typically follow a series of steps. First, they gather information about the patient's medical history and any potential triggers they might have been exposed to.
In most cases, the healthcare professional will examine the appearance and location of the rash. This can provide clues as to the type of dermatitis and potential causes. For example, contact dermatitis often presents as a red, itchy rash in specific areas where the skin has been in contact with an irritant or allergen.
There are various types of dermatitis, and the diagnostic process may involve the following:
Visual inspection: A direct examination of the skin helps determine the severity, patterns, and distribution of the rash.
Patch testing: In cases of suspected allergic contact dermatitis, patch testing can be used to identify specific irritants and allergens that may be causing the reaction. Small amounts of various substances are applied to the skin, and the reaction is observed after 48-72 hours.
Skin scraping or biopsies: If the cause or type of dermatitis is unclear, the healthcare professional may take a sample of the affected skin either through scraping or a biopsy. This can help rule out other skin conditions and identify the inflammation's underlying cause.
It is essential to remember that the diagnosis of dermatitis should be made by a healthcare professional and not self-diagnosed. Correct diagnosis ensures proper treatment, as different types of dermatitis may require various intervention methods.
General Treatment Approaches
When it comes to managing dermatitis, a combination of medical treatments and at-home care can help alleviate symptoms and prevent flare-ups. This section highlights both conventional medical approaches as well as helpful self-care practices.
Medical Treatments
Medical treatments for dermatitis primarily focus on reducing inflammation, itching, and moisture in the affected areas. Common medications prescribed for managing dermatitis include:
Topical creams and lotions: To soothe inflammation and itching, dermatologists often recommend over-the-counter hydrocortisone creams or prescription-strength corticosteroid creams. These may be applied to the affected areas as directed by a healthcare professional.
Oral antihistamines: Antihistamines such as diphenhydramine may be prescribed to help manage severe itching, particularly in cases of atopic dermatitis. It's essential to follow the recommended dose and seek medical advice if symptoms persist or worsen.
Prescription medications: In some cases, physicians may prescribe stronger medications like immunosuppressive drugs or biologic injections for more severe dermatitis. These should only be taken under the guidance and supervision of a qualified healthcare professional.
Self-Care and Home Remedies
In addition to medical treatments, several self-care practices and home remedies can help manage dermatitis symptoms and prevent flare-ups:
Moisturize regularly: Keeping the skin moisturized is crucial for soothing inflamed and itchy skin. Apply fragrance-free, gentle moisturizers at least twice a day, focusing on the affected areas.
Oatmeal baths: An oatmeal bath can help alleviate itching and redness associated with dermatitis. Add powdered colloidal oatmeal (how long does colloidal oatmeal last?) to lukewarm water and soak for 15-20 minutes. Gently pat the skin dry afterward and apply a moisturizer.
Use bath oils: Adding bath oils to your regular baths can help lock in moisture and soothe the skin. Make sure to choose a mild, fragrance-free oil suitable for sensitive skin.
Avoid irritants: Minimize contact with potential irritants such as harsh soaps, detergents, and chemicals. Opt for gentle, fragrance-free products specifically formulated for sensitive skin.
Keep cool: Excessive heat and sweat can exacerbate dermatitis symptoms, so stay cool during hot weather. Use a fan or air conditioner, and wear lightweight, breathable clothing.
By integrating these medical treatments and self-care practices into your routine, you can effectively manage dermatitis symptoms and work towards healthier, more comfortable skin. Remember to consult with a healthcare professional for personalized advice and recommendations.
Dermatitis and Skin Infections
Dermatitis is an umbrella term that describes a wide range of skin conditions characterized by inflammation, redness, and itching. Skin infections, mostly caused by bacteria, viruses, or fungi, can trigger dermatitis or aggravate existing skin conditions.
When the skin's natural barrier weakens, it becomes more susceptible to infections. In cases of atopic dermatitis, also known as eczema, the skin often lacks essential proteins and lipids, making it easier for pathogens to penetrate. Moreover, skin conditions like dermatitis create a favorable environment for bacterial growth due to the presence of moisture, which could lead to skin infections.
Some common skin infections associated with dermatitis are:
Impetigo: A highly contagious bacterial infection caused by Staphylococcus aureus or Streptococcus pyogenes. It presents as red sores that may discharge fluid and form a honey-colored crust.
Cellulitis: A bacterial infection of the skin's deeper layers, often caused by Staphylococcus or Streptococcus bacteria. It manifests as swollen, painful, and red skin areas that may emit warmth.
Fungal infections: Dermatophytes, the fungi causing ringworm, can thrive on skin affected by dermatitis. Additionally, yeast infections such as Candidiasis might result from a compromised skin barrier.
For individuals with dermatitis, preventing skin infections is crucial. Some measures to reduce the risk of infection include:
Practicing good hygiene, such as frequent hand washing and regular bathing with a gentle cleanser
Avoiding scratching, which can damage the skin and introduce bacteria
Managing stress as it can weaken the immune system and exacerbate dermatitis
Keeping the skin moisturized to maintain the skin barrier
Seeking prompt medical attention if signs of infection emerge
While dermatitis and skin infections can be uncomfortable and distressing, maintaining a strict skincare routine and taking preventative measures can significantly reduce their impact on one's daily life.
Dermatitis and Other Skin Conditions
Dermatitis is a common skin condition characterized by itchy, red, and inflamed skin. While there are various types of dermatitis, the symptoms often include rashes, scratching, and sensitive skin. In some cases, dermatitis can be mild, while in others, it may manifest as a more severe condition. Dermatitis shares similarities with other skin conditions; however, they each have distinct features that set them apart.
Rashes: Dermatitis often presents with redness and rashes, which may be itchy or painful. Other skin conditions like psoriasis and eczema also display rashes. However, dermatitis rashes typically appear in patches on exposed skin and can fluctuate in intensity during flare-ups.
Scratching: Itchy skin is a notable characteristic of dermatitis, leading to excessive scratching. This shared trait is also observed in conditions like hives or insect bite reactions. However, the itchiness in dermatitis is often more persistent and can cause further irritation or even infection if scratching continues.
Flare-ups: Similar to other chronic skin conditions, dermatitis may experience periods of flares and remission. Triggers for these flare-ups can vary and include irritants, allergens, or even stress. Identifying and avoiding triggers can help manage the frequency and severity of dermatitis symptoms.
Sensitive skin: Dermatitis sufferers often deal with sensitive skin, which can be easily irritated by external factors like harsh chemicals, heat, or friction. Other skin conditions, like rosacea or sunburn, may also involve sensitive skin but have different primary causes and presentations.
Moreover, dermatitis may lead to further complications like cracked skin if not properly managed. This condition is not unique to dermatitis, as other skin problems, such as psoriasis or extremely dry skin, can also result in cracked, painful skin.
In conclusion, dermatitis shares numerous features with other skin conditions, such as redness, itchiness, flare-ups, and sensitive skin. However, its specific triggers, presentation, and coexisting symptoms help to differentiate it from similar conditions. Understanding the similarities and differences is essential for proper diagnosis and treatment.
Tips for Prevention
Preventing dermatitis can be challenging, but there are some practical steps that can help reduce the risk of developing the condition. Implementing these preventive measures can promote overall skin health and protect against flare-ups.
Maintain a healthy skin barrier: Ensuring an intact and functional skin barrier is essential for preventing dermatitis. This can be achieved by:
Applying moisturizers regularly, especially after bathing or washing your hands
Using gentle and fragrance-free soap or cleansers
Avoiding prolonged contact with water or harsh chemicals
Wearing gloves when necessary to protect hands from irritants
Identify triggers and minimize exposure: Familiarizing yourself with common dermatitis triggers can help you avoid or minimize exposure to them. Triggers can vary, so it is essential to pay attention to the substances you come into contact with regularly. Some common triggers include:
Chemicals found in cleaning products or personal care items
Metals, such as nickel or cobalt
Fragrances and dyes in laundry detergents or cosmetics
Certain fabrics, like wool or synthetic materials
Stress, and anxiety can exacerbate symptoms
Extreme temperatures and humidity levels
Adopt a balanced diet: Eating nutrient-rich foods can contribute to overall skin health. Focus on consuming anti-inflammatory foods, such as:
Fruits and vegetables, especially leafy greens and berries
Omega-3 fatty acids found in fish, chia seeds (how long do chia seeds last?), and flaxseeds
Probiotics from yogurt, kefir, and fermented foods
Vitamins, minerals, and antioxidants from a wholesome diet
Create a skin-friendly environment: Modifying your surroundings can positively impact your skin's health. Consider implementing the following changes:
Maintain a consistent humidity level with a humidifier or dehumidifier
Use natural fabrics like cotton for bedding and clothing
Opt for fragrance-free laundry detergents and skincare products
Engage in relaxation techniques, such as meditation or yoga, to manage stress
By following these tips and prioritizing skin health, you can help to prevent dermatitis and enjoy healthier skin.
When to See a Dermatologist
Dermatitis, also commonly referred to as eczema, can often be managed at home with over-the-counter products and self-care measures. However, there are certain situations when it is essential to consult a dermatologist.
Seek professional help if you experience any of the following:
Persistent symptoms: If the symptoms of dermatitis, such as itchiness, redness, and swelling, do not improve with home remedies or over-the-counter treatments, it is advisable to see a dermatologist. They can diagnose the underlying cause and recommend an appropriate treatment plan.
Severe discomfort: Dermatitis can sometimes cause unbearable itchiness and pain, which can interfere with daily activities and sleep. A dermatologist can provide stronger prescription medications to alleviate these symptoms.
Signs of infection: If the affected skin appears infected, with increased redness, pus, or an unusual odor, it is essential to consult a dermatologist as soon as possible. An infection can spread to other areas of the body and may even lead to more serious health complications.
Fever: A fever, particularly if accompanied by other symptoms of infection, may indicate a more serious issue requiring a dermatologist's attention.
Multiple body parts affected: In some cases, dermatitis can affect multiple areas of the body, making self-management difficult. A dermatologist can help identify the cause and recommend a comprehensive treatment plan.
When visiting a dermatologist, be sure to provide them with a detailed history of your symptoms, any triggers you are aware of, and any treatments you have already tried. This information will help them to accurately diagnose the cause of your dermatitis and recommend the most effective treatment options for your specific situation.
In summary, consulting a dermatologist is crucial in specific cases of dermatitis when home remedies and over-the-counter treatments are not effective, or when the condition is accompanied by severe discomfort, infection, fever, or widespread symptoms. A dermatologist can provide specialized care and ensure a proper diagnosis and treatment plan.
#stasis dermatitis #atopic eczema #bacterial skin infections #viral skin infections #atopic dermatitis vary #skin diseases #severe eczema #irritant dermatitis