The Connection Between Grain-Free Diets and Autoimmune Diseases
Exploring the Link
Autoimmune diseases are conditions in which the immune system mistakenly attacks the body's own tissues, leading to inflammation, pain, and in many cases, chronic health issues. These diseases encompass a range of disorders, including celiac disease, type 1 diabetes, rheumatoid arthritis, and multiple sclerosis. The exact causes of autoimmune responses are complex and not fully understood, but both genetic and environmental factors, including diet, are believed to play significant roles. With the number of individuals affected by autoimmune diseases rising, researchers and patients alike are exploring dietary strategies to manage symptoms and potentially reduce disease activity.
Grain-free diets have garnered attention as a possible dietary intervention for those with autoimmune diseases. The elimination of grains, particularly those containing gluten like wheat, barley, rye, and oats, is a characteristic of such a diet. The rationale behind a grain-free diet for autoimmune disease management stems from the premise that certain proteins in grains could contribute to inflammation and autoimmunity. Celiac disease provides a clear example where the relationship between a gluten-containing diet and autoimmune response is well-established, necessitating a strict gluten-free diet for affected individuals.
Beyond celiac disease, there is ongoing research and debate as to whether a grain-free diet may benefit other autoimmune conditions. Some suggest that diets which reduce potential inflammatory foods, such as grains, could dampen the overall immune response, leading to an improvement in symptoms and possibly slowing disease progression. However, the scientific community has yet to reach a consensus, advocating for more rigorous studies to determine the efficacy and safety of grain-free diets in the context of various autoimmune diseases.
The connection between grain-free diets and autoimmune diseases is an area of growing interest and research, shedding light on the potential impact of dietary choices on autoimmune conditions. Understanding the effects of grains traditional modern diets and their potential relation to autoimmune diseases has led many individuals to explore the benefits of a grain-free diet.
For those seeking alternatives due to grain-free diabetes or incorporating grain-free pasta alternatives into their meals, a grain-free diet presents an opportunity to explore a wide range of flavorful and health-conscious options. Additionally, embracing a grain-free vegan lifestyle and delving into grain-free baking can offer a versatile and nourishing approach to nourishment.
The adoption of a grain-free diet has been associated with a variety of grain-free health benefits, and many individuals have shared inspiring grain-free success stories related to their autoimmune conditions. While more research is needed, the potential connection between grain-free diets and autoimmune diseases offers a promising avenue for individuals seeking to support their well-being through mindful dietary choices.
Understanding Autoimmune Diseases
Autoimmune diseases represent a significant health challenge due to their complexity and the body's own immune system initiating an attack on its tissue.
Definition and Classification of Autoimmune Diseases
Autoimmune diseases (ADs) arise when an individual's immune system erroneously targets and attacks normal cells within the body, unable to distinguish them from foreign invaders. Autoimmunity encompasses nearly 80 distinct diseases, ranging from systemic conditions like lupus and rheumatoid arthritis to organ-specific diseases, such as Type 1 diabetes and multiple sclerosis. Classification of these diseases is typically based on the primary tissues and organs affected, as well as the nature and pattern of symptoms.
Prevalence and Impact on Health
As a group, autoimmune diseases are common, affecting millions worldwide. They can have a pervasive impact on health, longevity, and quality of life. The prevalence of autoimmunity is significant – studies suggest it affects approximately 5-8% of the population. These diseases can be chronic, debilitating, and sometimes life-threatening, emphasizing the importance of understanding and managing these conditions.
Grain-Free Diets: Overview and Types
Grain-free diets exclude all cereal grains and products derived from them, which some individuals adopt due to health concerns, such as autoimmune diseases.
Components of Grain-Free Diets
A grain-free diet eliminates all grains, including wheat, barley, rye, and oats. It also avoids corn and rice, which are often considered staple grains in various cultures. Instead, the diet focuses on other food groups such as:
Meat and fish: primary sources of protein.
Vegetables: both leafy greens and root vegetables, excluding corn.
Fruits: all types, with attention to glycemic index as needed.
Dairy: included unless otherwise restricted by specific diet variations.
Eggs: a versatile protein source.
Legumes: providing plant-based protein and fiber.
Seeds and nuts: sources of healthy fats and proteins.
Tubers: such as sweet potatoes, provide a non-grain starch source.
Grain-free should not be confused with gluten-free; while all gluten-containing grains are excluded in a grain-free diet, gluten-free diets eliminate only gluten-containing grains but may include non-gluten grains like rice and corn.
Common Grain-Free Diet Variations
Several diet variations adopt grain-free principles, each with its own set of guidelines:
Paleo Diet: Excludes grains, legumes, and dairy, emphasizing whole foods that purportedly harken back to the Paleolithic era
Keto Diet: While not exclusively grain-free, it often results in grain exclusion due to its strict low-carb, high-fat macronutrient ratios
Autoimmune Protocol (AIP): An extension of Paleo designed to reduce inflammation and autoimmune disease symptoms, which eliminates grains and other potential irritants
Whole30: A 30-day program that cuts out grains along with sugar, alcohol, dairy, and legumes to reset eating patterns and identify food sensitivities
Proponents of grain-free diets often use gluten-free products as alternatives but carefully avoid grains like millet and other alternatives that may still contain types of starch or proteins considered problematic.
Scientific Research on Diet and Autoimmunity
Diet has been identified as a potential environmental factor that affects the incidence and progression of autoimmune diseases. Numerous studies have examined how specific diets, such as grain-free diets, may influence the autoimmune response.
Studies on Grain-Free Diets and Autoimmune Diseases
Researchers have explored the link between grain-free diets and autoimmune diseases by assessing the impact of these diets on the autoimmune response. The premise behind this research focuses on the possibility that grains could contribute to inflammation or an inappropriate immune response that leads to the production of antibodies targeting one's own tissues.
Study Observations: Some studies suggest that diets devoid of grains may help reduce the symptoms of autoimmune diseases. The reduction of grain consumption is theorized to possibly decrease the antigenic stimulus that might exacerbate the autoimmunity.
Study Impact on Autoimmunity Key Finding A Positive Reduction in antibodies associated with autoimmune diseases B Inconclusive No significant change in autoimmune response
Immune Response: A few studies have also explored how removing grains from one's diet affects intestinal health and, subsequently, the autoimmune response. The connection between gut health and systemic inflammation becomes imperative in understanding the onset and development of autoimmune diseases.
It remains important to approach the findings with a balanced view, acknowledging that while some individuals may report improvements with a grain-free diet, the results can vary widely. Moreover, a grain-free diet is restrictive and may not be suitable for everyone, as it can lead to nutritional deficiencies if not monitored and balanced carefully. Researchers continue to evaluate the broader implications and the long-term health effects of such diets.
The Gluten-Autoimmunity Connection
Gluten has been identified as a critical factor in the development and management of celiac disease and has been linked with other autoimmune conditions. This section delves into how gluten potentially evokes autoimmune responses and the specific conditions associated with its intolerance.
Gluten, Celiac Disease, and Autoimmune Conditions
Celiac disease is a notable autoimmune disorder where ingestion of gluten, a protein found in wheat, barley, and rye, triggers an immune response that damages the small intestine. Specifically, the gliadin and glutenin peptides in gluten are problematic. When these peptides are not completely digested, the resultant fragments can stimulate the production of anti-gliadin antibodies. In patients with celiac disease, this immune response doesn't just affect the gut; it can lead to systemic symptoms because these antibodies can target and damage other tissues and organs.
Key associations:
Autoimmune thyroid disease: A notable correlation exists where individuals with celiac disease are at increased risk of developing autoimmune thyroid conditions.
Autoimmune diabetes: Similarly, the risk of autoimmune diabetes, particularly type 1 diabetes, is higher in those with celiac disease, highlighting the connection between gluten intolerance and autoimmune disorders beyond the gastrointestinal tract.
Understanding Gluten's Role in Autoimmunity
The exact mechanism by which gluten exposure might lead to or exacerbate autoimmune diseases is complex. Gluten, particularly the peptide gliadin, has been hypothesized to contribute to autoimmunity through intestinal permeability, often referred to as "leaky gut." This permeability allows larger fragments of gliadin to enter the circulatory system, where they may be misidentified by the immune system as foreign invaders, leading to an inflammatory response.
In autoimmune diseases, this response can go awry, with the immune system mistakenly attacking the body's own cells. Thus, the connection between gluten and autoimmunity is an area of considerable interest and ongoing research.
Intestinal permeability and gliadin: Research suggests that gliadin may induce changes in intestinal permeability, thereby playing a pivotal role in the initiation of some autoimmune responses.
Anti-gliadin antibodies: The presence of these antibodies in individuals with gluten-related disorders points to an immune system that has become reactive not just to gluten but may erroneously target the body's own tissues.
Molecular Mimicry and Autoimmune Diseases
Molecular mimicry serves as a critical link in understanding how certain autoimmune diseases may develop in response to environmental triggers, including diet.
The Concept of Molecular Mimicry
Molecular mimicry occurs when proteins in foreign agents, such as food or pathogens, closely resemble the body’s own proteins, leading to an immune response that mistakenly targets the body’s own tissues. This biochemical mix-up is a key factor in the pathogenesis of various autoimmune conditions. Autoantibodies or autoreactive T cells are generated, both of which can attack host tissues believed to be foreign.
Molecular Mimicry and Specific Autoimmune Disorders
Multiple Sclerosis (MS): It is hypothesized that viral or bacterial antigens may mimic the myelin sheath, causing the immune system to attack the protective covering of nerves, leading to neurological symptoms.
Rheumatoid Arthritis (RA): Shared epitopes between the synovial joint fluid and bacterial proteins might activate T cells that attack joint tissue.
Lupus (SLE): Molecular mimicry might contribute to the production of antibodies against self-antigens, including nuclear components, causing systemic effects.
Psoriasis: Streptococcal infections have been implicated in triggering psoriatic lesions via molecular mimicry.
Hashimoto's Thyroiditis: A common thyroid disorder, might be initiated by a viral or bacterial protein resembling thyroid gland components, prompting an immune attack on the gland.
Graves' Disease: Similarly to Hashimoto's, the immune system might target the thyroid, leading to overactivity based on mimicry mechanisms.
Pemphigus Vulgaris: Desmoglein (a component of skin cells) can be mistaken for foreign antigens, resulting in blistering skin diseases.
The role of grain-free diets in this context involves the potential for dietary proteins to act as mimics, highlighting the importance of dietary choices in managing autoimmune diseases.
The Immunological Response to Diet
The connection between diet and the immune system is complex, with particular attention to how grain-free diets may influence autoimmune disease development. Dietary proteins, once digested, enter systemic circulation as amino acids, which may affect the body's immunological responses.
Digestion and Systemic Circulation of Amino Acids
Protein digestion begins within the stomach and continues in the small intestine, where proteolytic enzymes break proteins down into amino acids. These amino acids are then absorbed into the bloodstream through the intestinal wall. Systemic circulation distributes these nutrients throughout the body, where they can become the building blocks for various bodily functions, including the synthesis of immune cells. In individuals with autoimmune conditions, such as autoimmune thyroid disease or autoimmune diabetes, the intake and circulation of specific amino acids could potentially influence disease pathways.
Immunoglobulins and Diet-Induced Autoimmunity
Immunoglobulins (antibodies) are proteins produced by the immune system to recognize and neutralize pathogens. Diet can modify the immune response, potentially triggering an imbalance or misdirection of this system. For instance, a grain-free diet may alter the immune system's response, sometimes leading to diet-induced autoimmunity. This occurs when the immune system mistakenly targets the body's own cells, which is characteristic of conditions like autoimmune thyroid disease. The role of diet, especially as it pertains to the levels of immunoglobulins, is a significant factor in understanding and managing autoimmune diseases.
The Role of Intestinal Permeability in Autoimmune Diseases
Intestinal permeability, commonly known as "leaky gut," contributes notably to the development of autoimmune diseases by allowing substances into the bloodstream that can trigger an immune response.
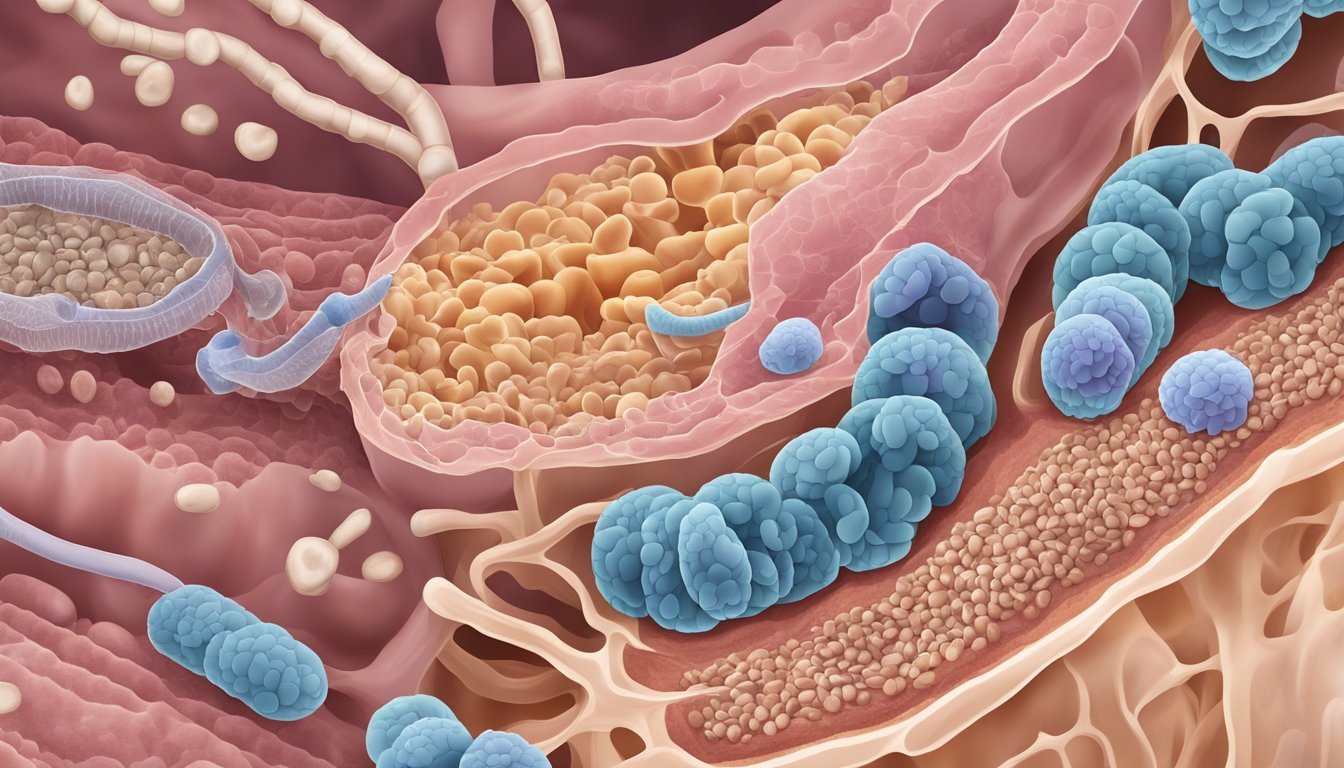
Gut Microbiota and Autoimmune Diseases
The gut microbiota is a complex community of microorganisms that live in the digestive tracts of humans. This community plays a crucial role in maintaining gut integrity and immune system balance. Imbalances in gut microbiota, known as dysbiosis, can lead to increased intestinal permeability, where the mucosal barrier becomes compromised. This allows particles such as bacteria and toxins to pass from the gut into the circulation. Such breaches in the barrier can lead to an immune response, which, in susceptible individuals, may contribute to the development of autoimmune diseases like Hashimoto’s thyroiditis.
Mucosal Changes: The interaction of pathogenic microorganisms with the gut-associated lymphoid tissue can induce mucosal changes, leading to a self-perpetuating cycle of inflammation and tissue damage in autoimmune conditions.
Enterocytes: These cells, lining the gut, can be affected by dysbiosis, compromising their role in barrier function and leading to heightened gut permeability.
Diet and Its Impact on Gut Permeability
Diet plays an influential role in modulating gut permeability. In particular, the consumption or exclusion of certain components—like prolamins found in gluten-containing grains—may affect the integrity of the gut lining.
Zonulin: This protein modulates the tight junctions between enterocytes in the gut. Certain dietary components, specifically prolamins, can stimulate zonulin release, which increases intestinal permeability. For individuals with autoimmune diseases, this can exacerbate symptoms.
Mucosal Recovery: A grain-free diet may help promote mucosal recovery by removing potential triggers that can increase gut permeability.
Beneficial Diet Practices:
Reducing foods that trigger zonulin release, which may decrease gut permeability.
Including nutrients that support mucosal health and integrity.
The viability of a grain-free diet to improve autoimmune disease symptoms through the reduction of intestinal permeability remains a subject of ongoing research. However, the link between a compromised gut and autoimmune reactions is an area of high significance in understanding these complex disorders.
Dietary Management of Autoimmune Conditions
Managing autoimmune conditions often involves a tailored diet aimed at reducing inflammation and immune system volatility. Key strategies include the introduction of hypoallergenic foods and specific dietary frameworks that support improved health outcomes for those with autoimmune diseases.
Hypoallergenic Foods and Autoimmunity
Hypoallergenic foods play a crucial role in managing autoimmune conditions as they are less likely to trigger an immune response. Sorghum, for instance, is a gluten-free grain and a member of the panicoid family. It serves as an excellent hypoallergenic alternative to wheat. Sorghum's benefits are particularly relevant for individuals with food protein-induced enterocolitis syndrome (FPIES), a condition involving severe hypersensitivity to food proteins. These grains help maintain intestinal barrier function, which is vital for patients with autoimmune diseases, by preventing the passage of harmful substances that could trigger an immune response.
Orzenin, a rice protein, is another hypoallergenic alternative, often considered in dietary management. By including such foods that are less likely to provoke the immune system, individuals can potentially avoid exacerbating symptoms associated with their autoimmune conditions.
Dietary Strategies for Autoimmune Disease Management
A systematic approach to dietary management can help in controlling the manifestation of autoimmune diseases. Grain-free diets have been suggested as a method to alleviate autoimmune symptoms, especially in those with gluten sensitivities or celiac disease where gluten can cause inflammation and damage to the intestinal lining.
However, it's critical to ensure nutritional adequacy when excluding major food groups like grains. Here is a table that outlines rational decisions in dietary strategies for autoimmune disease management:
Strategy Implications for Autoimmune Conditions Considerations Elimination of gluten-containing grains Potentially reduces inflammation and immune response Balance diet with gluten-free grains such as sorghum Inclusion of hypoallergenic food sources Lowers chance of triggering immune response Choose alternatives like sorghum or rice-based proteins Maintenance of intestinal barrier function Prevents unwanted immune activations Incorporate foods that support gut health and integrity
A personalized approach to diet, taking into account individual sensitivities and nutritional needs, is critical in the management of autoimmune conditions. Through these specific dietary strategies, individuals may be able to reduce symptoms and improve their overall well-being.
Conclusion
This section encapsulates the understanding of how grain-free diets may interact with autoimmune conditions and looks ahead to the potential for further research.
Summary of Connections
Research indicates immunoreactivity to certain grain components might exacerbate autoimmune responses, affecting conditions like thyroid peroxidase autoantibody production in autoimmune thyroid diseases or the inflammation seen in psoriatic arthritis. Specific diets that eliminate grains are suggested to benefit individuals by reducing these immune reactions. In adults with autoimmune conditions, grain-free diets have been correlated with symptom relief and potentially improved gut health, as grains can affect enterocytes, which are integral to intestinal barrier function. It is important to note that the evidence does not suggest a direct correlation with mortality rates or the prevalence of conditions such as autism.
Future Directions in Research and Treatment
The field beckons for comprehensive studies to solidify the role of grain-free diets in the management of autoimmune diseases. There are opportunities to explore:
Longitudinal Studies: To assess long-term efficacy and safety of grain-free diets in adults with autoimmune conditions.
Mechanistic Research: To understand how elimination of grains influences immunoreactivity at the cellular level, including effects on enterocytes.
Diverse Population Sampling: To ensure findings are applicable across diverse genetic backgrounds and conditions, such as psoriatic arthritis and autoimmune thyroid disorders.
By advancing this research, healthcare professionals may develop more nuanced guidelines for dietary interventions as part of an integrated treatment plan for autoimmune diseases.