Balanced Type 2 Diabetes Meal Plan
A Week of Nutritious and Delicious Eating
Managing type 2 diabetes requires careful attention to diet and nutrition. A well-planned meal strategy can help control blood sugar levels, promote weight loss, and improve overall health. A diabetes meal plan typically includes a balanced mix of carbohydrates, proteins, and healthy fats, with an emphasis on whole foods and portion control.
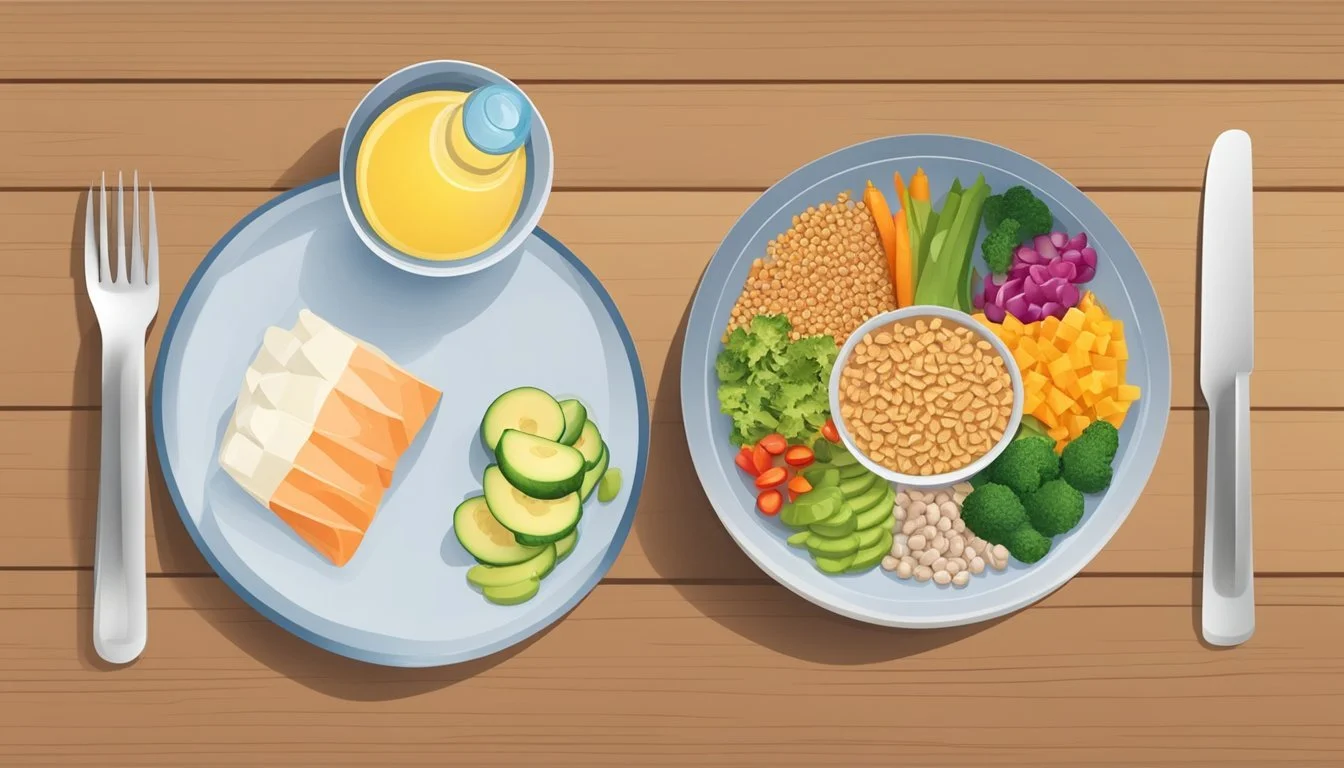
Creating a diabetes-friendly meal plan doesn't have to be complicated. The American Diabetes Association recommends using the Diabetes Plate Method as a simple guide. This approach involves filling half the plate with non-starchy vegetables, a quarter with lean protein, and the remaining quarter with carbohydrates. Regular meal timing is also important, allowing 2-3 hours between meals for blood glucose to stabilize.
Incorporating a variety of nutrient-dense foods into the diet can make meal planning more enjoyable and sustainable. Colorful vegetables, whole grains, lean meats, fish, and plant-based proteins offer both essential nutrients and satisfying flavors. By focusing on these wholesome choices and minimizing processed foods and added sugars, individuals with type 2 diabetes can better manage their condition while still enjoying delicious meals.
Understanding Type 2 Diabetes
Type 2 diabetes is a chronic condition affecting how the body processes glucose. Proper management requires knowledge of blood sugar control and working closely with a healthcare team.
What Is Type 2 Diabetes?
Type 2 diabetes occurs when the body becomes resistant to insulin or doesn't produce enough insulin. This leads to high blood sugar levels, which can cause serious health complications if left untreated.
Risk factors include obesity, physical inactivity, age, and family history. Symptoms may develop gradually and include increased thirst, frequent urination, blurred vision, and slow-healing wounds.
Diagnosis typically involves blood tests to measure glucose levels. Early detection and treatment are crucial for preventing complications like heart disease, kidney damage, and nerve problems.
Blood Sugar Control Fundamentals
Maintaining healthy blood sugar levels is essential for managing type 2 diabetes. The target range varies by individual, but generally aims for 80-130 mg/dL before meals and less than 180 mg/dL two hours after eating.
Regular blood glucose monitoring helps track progress and inform treatment decisions. This may involve using a home glucose meter or continuous glucose monitor.
Diet plays a key role in blood sugar control. A balanced meal plan focuses on:
Whole grains
Lean proteins
Non-starchy vegetables
Healthy fats
Limited added sugars
Physical activity also helps regulate blood sugar by improving insulin sensitivity. Aim for at least 150 minutes of moderate exercise per week.
Medication may be necessary to supplement lifestyle changes. Options include metformin, sulfonylureas, and insulin therapy.
The Basics of a Diabetes 2 Meal Plan
A well-structured meal plan is crucial for managing type 2 diabetes. It helps control blood sugar levels and supports overall health through balanced nutrition.
The Role of Nutrition in Diabetes Management
Proper nutrition plays a vital role in managing type 2 diabetes. A balanced meal plan helps regulate blood glucose levels and maintain a healthy weight.
Eating regular meals at consistent times is key. This approach prevents large fluctuations in blood sugar throughout the day.
Focus on whole, unprocessed foods. Include a variety of colorful vegetables, lean proteins, whole grains, and healthy fats in your meals. These nutrient-dense choices provide essential vitamins and minerals.
Portion control is equally important. Use the plate method as a guide: fill half your plate with non-starchy vegetables, a quarter with lean protein, and a quarter with whole grains or starchy vegetables.
Macronutrients and Blood Sugar
Understanding how different macronutrients affect blood sugar is essential for meal planning. Carbohydrates have the most significant impact on blood glucose levels.
Carbohydrates:
Choose complex carbs like whole grains, legumes, and vegetables
Limit refined carbs and added sugars
Aim for consistent carb intake at each meal
Protein:
Helps stabilize blood sugar
Choose lean sources like fish, poultry, and plant-based options
Fats:
Focus on healthy fats from sources like avocados, nuts, and olive oil
Limit saturated and trans fats
Fiber:
Slows digestion and helps control blood sugar spikes
Aim for 25-30 grams per day from fruits, vegetables, and whole grains
Balancing these macronutrients in each meal helps maintain steady blood glucose levels throughout the day.
Creating Your Meal Plan
Effective meal planning is crucial for managing type 2 diabetes. A well-structured plan helps maintain stable blood sugar levels and supports overall health.
Meal Planning Techniques
Start by setting clear goals for your eating plan. Consider your dietary preferences, lifestyle, and any medications you take. Choose from seven recommended meal patterns for diabetes management. These include Mediterranean, low-carb, vegetarian, and flexible carbohydrate approaches.
Create a weekly menu to simplify grocery shopping and meal preparation. Include a variety of nutrient-dense foods like fruits, vegetables, whole grains, and lean proteins. Plan for three balanced meals and two to three snacks daily to maintain steady blood sugar levels.
Adjust your meal plan as needed based on blood glucose readings and hunger levels. Regularly consult with a registered dietitian to fine-tune your approach and address any challenges.
Portion Control and The Plate Method
The Diabetes Plate method is an easy-to-use tool for creating balanced meals. Fill half your plate with non-starchy vegetables, one quarter with lean protein, and one quarter with carbohydrates.
Use measuring cups or a food scale to ensure proper serving sizes. Common portion control aids include:
Your palm for protein servings
Your fist for fruit or vegetable servings
Your thumb tip for fats like oils or butter
Pay attention to food labels to understand serving sizes and carbohydrate content. Be mindful of hidden sugars and fats in packaged foods.
Gradually reduce portion sizes if needed for weight management. This approach allows for sustainable changes without feeling deprived.
What to Eat
A diabetes-friendly meal plan focuses on nutrient-dense foods that help manage blood sugar levels. It emphasizes quality carbohydrates, lean proteins, healthy fats, and plenty of vegetables.
Choosing Quality Carbohydrates
Opt for complex carbohydrates that are high in fiber and nutrients. Whole grains like quinoa, brown rice, and oatmeal are excellent choices. They provide sustained energy and help control blood glucose levels.
Legumes such as lentils, chickpeas, and black beans are rich in fiber and protein. These can be incorporated into soups, salads, or as side dishes.
Limit refined carbohydrates like white bread, pasta, and sugary snacks. These can cause rapid spikes in blood sugar. Instead, choose whole grain alternatives when possible.
Incorporating Proteins and Healthy Fats
Lean proteins are essential for maintaining muscle mass and promoting satiety. Choose options like skinless chicken, fish, tofu, and lean cuts of beef or pork.
Eggs are a versatile protein source that can be enjoyed at any meal. They're packed with nutrients and have minimal impact on blood sugar.
Healthy fats from sources like avocados, olive oil, and nuts are important for hormone balance and nutrient absorption. Include small portions of these in your meals.
Greek yogurt is high in protein and can be a great snack or breakfast option. Choose plain varieties and add your own fresh fruit for flavor.
Selecting Fruits and Vegetables
Non-starchy vegetables should make up a large portion of your plate. Broccoli, spinach, kale, and bell peppers are nutrient-dense options that are low in carbohydrates.
Aim for a variety of colorful vegetables to ensure a wide range of vitamins and minerals. Roast, steam, or enjoy them raw in salads.
Fruits can be part of a diabetes meal plan, but portion control is key. Berries, apples, and citrus fruits are good choices due to their lower sugar content and high fiber.
Limit fruit juices, as they lack fiber and can cause rapid blood sugar spikes. Whole fruits are always a better option.
Recipes and Food Ideas
A diabetes-friendly meal plan includes a variety of nutritious and delicious options for every meal and snack. These recipes focus on balanced nutrition while keeping blood sugar levels stable.
Breakfast Options
Start the day with protein-rich Greek yogurt topped with sliced apple and a sprinkle of cinnamon. For a savory option, try a spinach and cheese omelet with whole-grain toast. Overnight oats made with almond milk, chia seeds, and berries offer a convenient grab-and-go breakfast.
Whole-grain pancakes topped with sugar-free syrup and a side of turkey bacon provide a satisfying weekend treat. A smoothie bowl made with unsweetened almond milk, frozen berries, and a scoop of protein powder offers a refreshing start to the day.
Lunch Suggestions
A turkey and avocado wrap using a low-carb tortilla makes for a quick and easy lunch. Pair it with cucumber slices and hummus for added crunch and fiber. A large salad with mixed greens, grilled chicken, feta cheese, and a light vinaigrette dressing is both filling and nutritious.
Lentil soup with a side of whole-grain crackers provides warmth and comfort on chilly days. For a Mediterranean-inspired meal, try a Greek salad with cucumbers, tomatoes, olives, and feta cheese, topped with grilled salmon.
Dinner Inspiration
Baked salmon with roasted vegetables like Brussels sprouts and sweet potatoes offers a balanced and flavorful dinner. Lean beef stir-fry with broccoli, bell peppers, and snow peas over cauliflower rice is a low-carb alternative to traditional takeout.
Grilled chicken breast seasoned with herbs, served alongside a quinoa pilaf and steamed green beans, provides a well-rounded meal. For a vegetarian option, try stuffed bell peppers filled with a mixture of quinoa, black beans, and vegetables, topped with a small amount of cheese.
Snack and Dessert Choices
Apple slices with almond butter make for a satisfying snack that combines fiber and protein. Hard-boiled eggs paired with cherry tomatoes offer a protein-packed option to curb hunger between meals. For a crunchy treat, try air-popped popcorn seasoned with herbs.
Greek yogurt parfaits layered with berries and a sprinkle of nuts provide a sweet yet nutritious dessert. Sugar-free gelatin topped with a dollop of whipped cream satisfies sweet cravings without spiking blood sugar. Frozen grapes offer a refreshing, naturally sweet treat on hot days.
Meal Prepping and Tips
Effective meal planning and preparation are key for managing type 2 diabetes. Smart strategies can save time, ensure balanced nutrition, and help maintain stable blood sugar levels.
Efficient Meal Prep Strategies
Batch cooking is a time-saving technique for diabetes management. Cook large portions of lean proteins, whole grains, and vegetables to use throughout the week. Store prepped ingredients in portion-controlled containers for easy assembly.
Create a weekly meal plan focusing on balanced nutrition. Include a variety of nonstarchy vegetables like kale and edamame. Pair these with lean proteins and complex carbohydrates such as brown rice.
Use slow cookers or instant pots for hands-off meal preparation. These appliances are great for making soups, stews, and one-pot meals rich in nutrients and fiber.
Pre-portion snacks into small containers to avoid overeating. Mix nuts, seeds, and dried fruits for a nutrient-dense option. Keep cut vegetables readily available for quick, low-carb snacking.
Smart Shopping for Diabetes
Plan grocery trips around your meal prep schedule. Make a detailed shopping list to avoid impulse purchases and ensure you have all necessary ingredients.
Focus on whole foods in the perimeter of the store. Choose colorful fruits and vegetables, lean meats, and dairy products. These foods are typically lower in added sugars and higher in essential nutrients.
Read nutrition labels carefully. Pay attention to serving sizes, total carbohydrates, and fiber content. Look for products with minimal added sugars and saturated fats.
Stock up on healthy fats like olive oil and foods rich in omega-3 fatty acids. These can help improve insulin sensitivity and reduce inflammation.
Experiment with herbs and spices to add flavor without extra calories or carbs. They can make meals more satisfying without impacting blood sugar levels.
Managing Your Diet in Daily Life
Living with diabetes requires consistent dietary management. Key strategies include planning ahead, making smart food choices, and adapting to different social situations.
Eating Out with Diabetes
Dining out can be enjoyable while managing diabetes. Research restaurant menus in advance to find diabetes-friendly options. Choose grilled, baked, or steamed dishes instead of fried foods. Ask for dressings and sauces on the side to control portions.
Opt for vegetable-based sides rather than white pasta or bread. Request substitutions like a salad instead of fries. Be mindful of portion sizes - consider sharing an entrée or taking half home.
Don't hesitate to ask about ingredients or preparation methods. Many restaurants are accommodating to dietary needs. Stay hydrated with water or unsweetened beverages. Limit alcohol consumption, as it can affect blood sugar levels.
Navigating Social Situations
Social events often revolve around food, but they don't have to derail diabetes management. Eat a small, balanced snack before attending gatherings to avoid overeating. Bring a diabetes-friendly dish to share at potlucks.
Focus on socializing rather than food. Position yourself away from the buffet or snack table to reduce temptation. Choose wisely from available options - fill half your plate with non-starchy vegetables.
Be prepared to politely decline food offers that don't fit your meal plan. True friends will understand and support your health goals. If alcohol is served, opt for lower-carb choices like dry wine or spirits with sugar-free mixers.
Adjusting Your Meal Plan
A diabetes meal plan requires regular adjustments to maintain optimal blood sugar control. Flexibility and personalization are key to long-term success in managing diabetes through nutrition.
Review and Revise Based on Results
Monitor blood sugar levels regularly and track how different foods affect them. Keep a food diary to identify patterns. If blood sugar consistently runs high after certain meals, reduce portion sizes or swap out high-glycemic foods. For low blood sugar, add small amounts of carbohydrates or adjust medication timing.
Look for trends over time. Gradual changes in weight, activity level, or medication may necessitate meal plan updates. The American Diabetes Association recommends reviewing your plan every 3-6 months.
Consider using a continuous glucose monitor for more detailed insights into how specific foods impact blood sugar. This data can guide precise meal plan refinements.
Collaborate with Your Health Care Team
Schedule regular check-ups with your doctor and registered dietitian. Bring your food and blood sugar logs to appointments. Discuss any challenges or concerns with your current meal plan.
Your health care team can help interpret your results and suggest evidence-based adjustments. They may recommend changes to meal timing, carbohydrate distribution, or specific food choices based on your individual needs and goals.
Be open about your lifestyle and preferences. Your team can help tailor your plan to fit your schedule, budget, and food preferences while still meeting nutritional targets. They can also advise on adjusting your meal plan for special situations like travel or illness.