Master the Diabetes Plate Method: Your Guide to Balanced, Blood Sugar-Friendly Meals
Managing diabetes through diet can be challenging, but the diabetes dinner plate method simplifies meal planning. This approach helps individuals create balanced, portion-controlled meals without complex calculations or measurements.
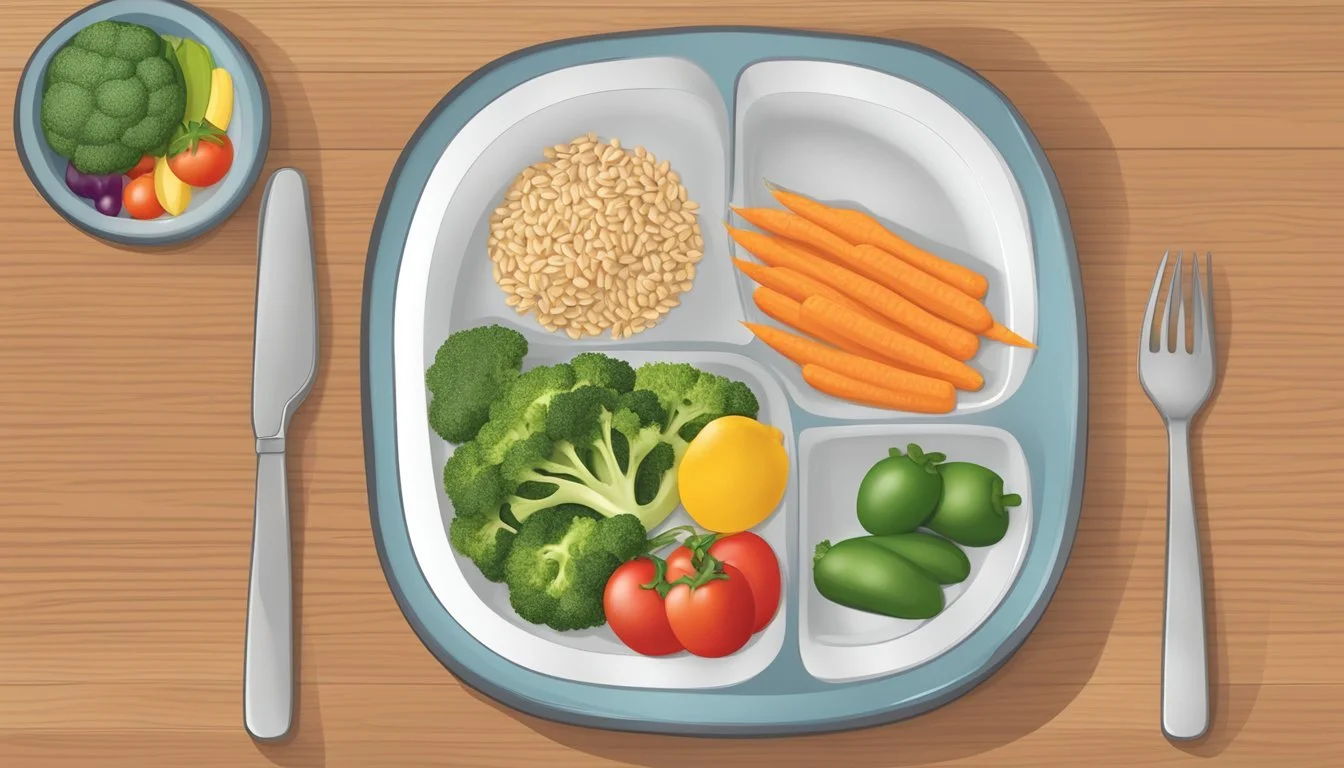
The diabetes plate method divides a 9-inch plate into sections: half for non-starchy vegetables, one-quarter for lean protein, and one-quarter for carbohydrates. This visual guide promotes a healthy balance of nutrients while helping to regulate blood sugar levels. By following this method, people with diabetes can enjoy satisfying meals that support their health goals.
Implementing the diabetes plate method is straightforward and adaptable to various cuisines and preferences. It encourages the consumption of nutrient-dense foods and provides flexibility in meal choices. The simplicity of this approach makes it an effective tool for long-term diabetes management and overall healthy eating habits.
Understanding the Diabetes Plate Method
The Diabetes Plate Method offers a simple, visual approach to creating balanced meals for managing blood sugar. It provides guidance on portion sizes and food group ratios without complex counting or measuring.
The Basics of Plate Method
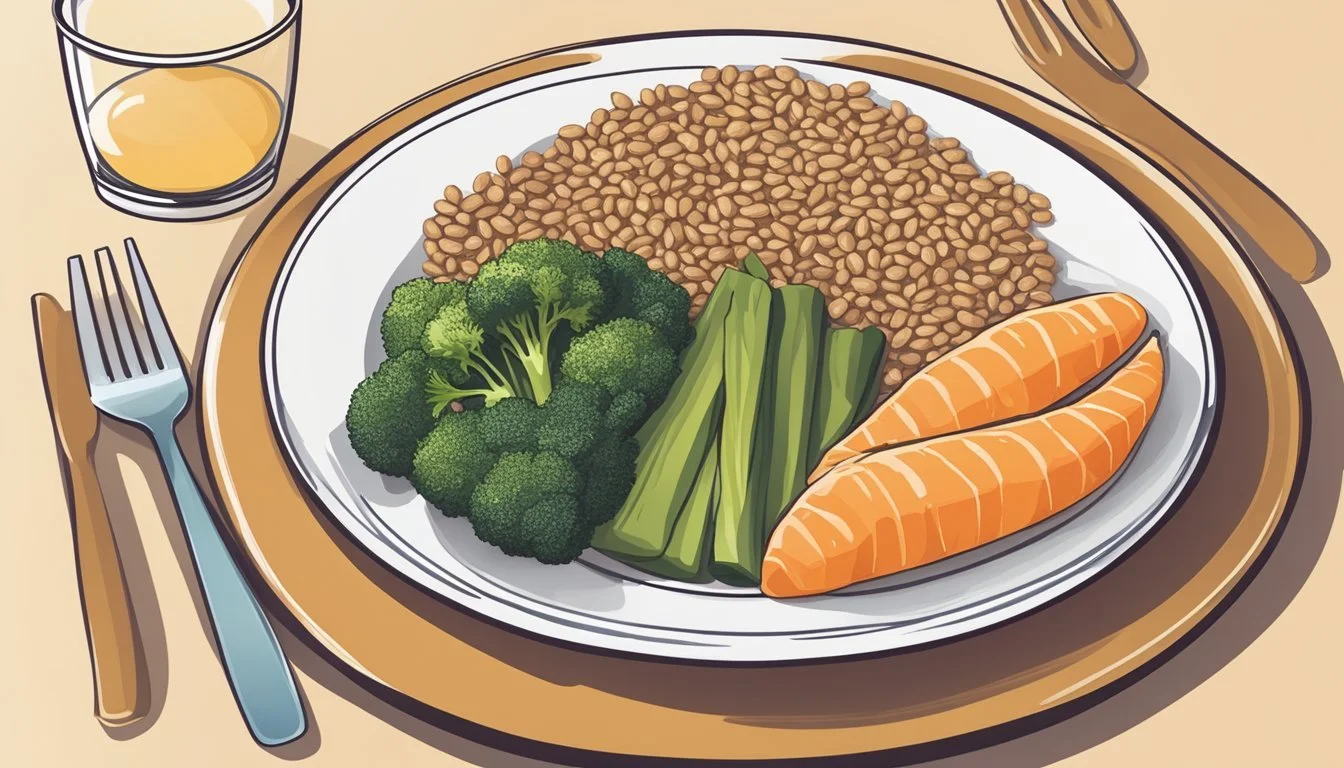
The Diabetes Plate Method uses a standard 9-inch dinner plate as a guide. Fill half the plate with non-starchy vegetables like broccoli, carrots, or salad greens. Reserve one quarter for lean protein sources such as chicken, fish, or tofu. The remaining quarter is for carbohydrate foods like whole grains, starchy vegetables, or fruit.
This method eliminates the need for strict calorie counting or carbohydrate tracking. It provides a quick, easy way to ensure balanced nutrition at each meal. The visual nature of the plate method makes it accessible for people of all ages and backgrounds.
Benefits for Blood Glucose Management
The Diabetes Plate Method helps regulate blood glucose levels by promoting balanced meals. By limiting carbohydrates to one quarter of the plate, it reduces the risk of blood sugar spikes after eating. The emphasis on non-starchy vegetables increases fiber intake, which can slow digestion and help stabilize blood sugar.
This approach also supports weight management, a key factor in diabetes control. The large portion of low-calorie vegetables promotes feelings of fullness while keeping overall calorie intake in check. Consistent use of the plate method can lead to improved glycemic control and potentially reduced need for medication in some individuals with diabetes.
Creating a Balanced Dinner Plate
The diabetes plate method offers a simple approach to building nutritious meals that help manage blood sugar levels. It focuses on proper proportions of key food groups and selecting quality ingredients.
Proportioning Macronutrients
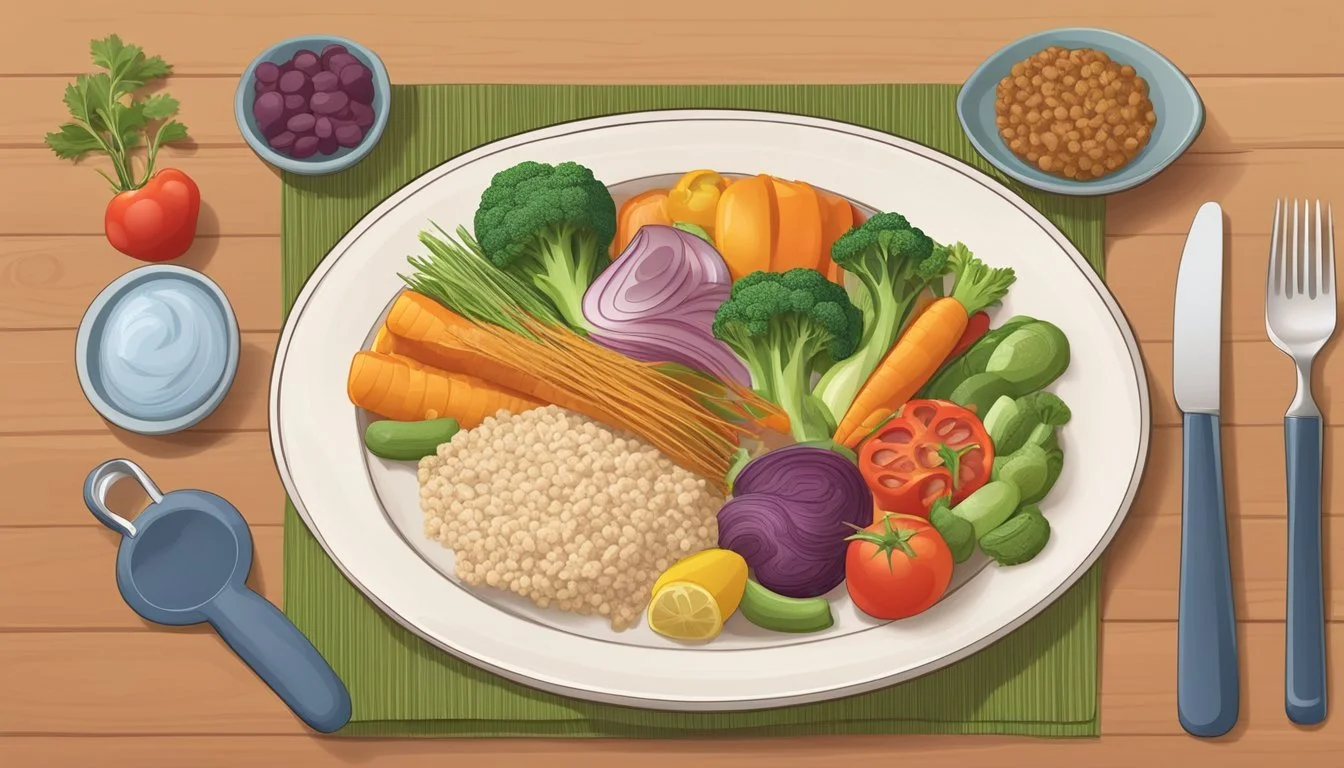
Fill half the plate with non-starchy vegetables like leafy greens, broccoli, or peppers. These provide essential nutrients and fiber while having minimal impact on blood sugar.
Reserve one quarter for lean proteins such as chicken, fish, tofu, or beans. Protein helps maintain muscle mass and promotes satiety.
The remaining quarter is for carbohydrate foods. Choose whole grains, starchy vegetables, or fruit. These provide energy and important nutrients.
Add small amounts of healthy fats like olive oil, avocado, or nuts. Fats slow digestion and help absorb fat-soluble vitamins.
Choosing Quality Foods
Select nutrient-dense, minimally processed options. Opt for whole grains over refined carbs. Brown rice, quinoa, and whole wheat bread offer more fiber and nutrients.
Choose a variety of colorful vegetables. Different colors indicate diverse nutrients and antioxidants. Aim for at least 3-5 servings daily.
Pick lean proteins low in saturated fat. Skinless poultry, fish, and plant-based proteins are excellent choices. Limit red meat to occasional servings.
Include heart-healthy fats from sources like olive oil, nuts, and fatty fish. These support overall health and help manage blood sugar levels.
Essential Components of a Diabetes-Friendly Meal
A balanced diabetes-friendly meal focuses on nutrient-dense foods that support blood sugar management. Key components include fiber-rich options, lean proteins, and healthy fats.
Incorporating High-Fiber Choices
Fiber plays a crucial role in diabetes management. Non-starchy vegetables should fill half the plate. These include leafy greens, broccoli, cauliflower, and bell peppers. They provide essential nutrients and help slow digestion.
Whole grains are another excellent fiber source. Options like quinoa, brown rice, and whole wheat pasta can occupy a quarter of the plate. Legumes such as lentils and chickpeas offer both fiber and protein.
Fruits can be included in moderation. Berries, apples, and pears are good choices due to their lower glycemic impact and high fiber content.
Selecting Healthy Sources of Protein
Lean proteins should make up about a quarter of the plate. They help maintain muscle mass and provide satiety without significantly impacting blood sugar levels.
Good options include:
Skinless chicken or turkey breast
Fish (salmon, tuna, cod)
Lean cuts of beef or pork
Eggs
Tofu and tempeh
Plant-based proteins like beans and lentils can serve as both protein and fiber sources. Greek yogurt offers protein while providing probiotics for gut health.
Understanding Fats and Their Role
While fats don't directly affect blood sugar, they impact overall health and diabetes management. Focus on heart-healthy unsaturated fats.
Include sources like:
Avocados
Nuts and seeds
Olive oil
Fatty fish (salmon, mackerel, sardines)
These fats can help reduce inflammation and improve insulin sensitivity. They also aid in the absorption of fat-soluble vitamins.
Limit saturated and trans fats found in fried foods, full-fat dairy, and processed snacks. These can contribute to insulin resistance and cardiovascular issues.
Meal Planning Strategies for Diabetes
Effective meal planning is crucial for managing diabetes. A structured approach helps maintain stable blood sugar levels and promotes overall health.
Daily Meal Planning Tips
Use the Diabetes Plate Method to simplify meal creation. Fill half the plate with non-starchy vegetables like salad, green beans, or broccoli. Dedicate one quarter to lean protein such as chicken, tofu, or eggs. Reserve the final quarter for carbohydrate-rich foods like whole grains or starchy vegetables.
Plan meals around vegetables to ensure proper nutrition. Incorporate a variety of colorful produce to maximize nutrient intake. Balance carbohydrates throughout the day to avoid blood sugar spikes.
Create a weekly meal schedule. This reduces decision fatigue and helps maintain consistency. Include snacks in the plan to prevent hunger-driven poor choices.
Long-Term Strategies for Success
Build a recipe collection tailored to diabetes management. Explore diabetes-friendly cookbooks or online resources like the Diabetes Food Hub for inspiration. Adapt favorite recipes by substituting ingredients or adjusting portion sizes.
Develop a rotating meal schedule. This ensures variety while simplifying planning. Include 2-3 options for each meal to prevent boredom.
Practice batch cooking. Prepare larger quantities of staple items like grilled chicken or roasted vegetables. Store portioned meals for quick, balanced options throughout the week.
Learn to read nutrition labels effectively. Focus on total carbohydrates, fiber content, and serving sizes. This skill aids in making informed food choices and maintaining glycemic control.
Suggested Dinner Foods for Diabetes
Planning diabetes-friendly dinners involves choosing nutrient-dense foods that help manage blood sugar levels. The plate method provides a simple framework for creating balanced meals.
Lean Meats and Plant-Based Proteins
Lean meats and plant-based proteins are essential components of a diabetes-friendly dinner plate. They provide satiety without significantly impacting blood glucose.
Grilled chicken breast, turkey, and fish like salmon or cod are excellent lean meat options. For plant-based alternatives, consider:
Tofu
Tempeh
Lentils
Chickpeas
Black beans
A 3-ounce serving of cooked lean protein should occupy about 1/4 of the dinner plate. These proteins can be prepared in various ways, such as baking, grilling, or sautéing with minimal added fats.
Non-Starchy Vegetables for Nutrient Density
Non-starchy vegetables should fill half the dinner plate. They are low in carbohydrates and high in fiber, vitamins, and minerals.
Recommended non-starchy vegetables include:
Leafy greens (spinach, kale, arugula)
Broccoli
Cauliflower
Bell peppers
Asparagus
Green beans
Tomatoes
Mushrooms
These vegetables can be steamed, roasted, or eaten raw in salads. Aim for a variety of colors to ensure a wide range of nutrients.
Whole Grains and Starchy Vegetables in Moderation
The remaining quarter of the plate can include whole grains or starchy vegetables. These foods provide essential carbohydrates but should be consumed in moderation.
Whole grain options:
Quinoa
Brown rice
Whole wheat pasta
Barley
Starchy vegetables:
Sweet potatoes
Corn
Green peas
Portion control is crucial for these foods. A serving size is typically 1/2 cup for cooked grains or starchy vegetables. Whole grains are preferred over refined grains due to their higher fiber content, which helps slow down blood sugar absorption.
Dinner Recipes and Cooking Tips
Crafting diabetes-friendly dinners involves adapting recipes and using cooking methods that retain nutrients. These strategies help create balanced, flavorful meals that align with the diabetes plate method.
Recipe Adaptations for Diabetes
Modifying recipes for diabetes focuses on balancing nutrients and controlling portion sizes. Replace refined grains with whole grains in dishes like pasta or rice. Swap full-fat dairy for low-fat options in creamy sauces or casseroles.
Reduce added sugars by using natural sweeteners or fruit purees. Incorporate more non-starchy vegetables to increase fiber and nutrients without significantly impacting blood sugar.
For protein, choose lean meats, fish, or plant-based options like beans and lentils. Use herbs and spices to enhance flavor without adding salt or sugar.
Cooking Methods to Retain Nutrients
Steaming vegetables preserves vitamins and minerals better than boiling. Roasting brings out natural flavors without added fats.
Grilling meats allows excess fat to drip away. Use a marinade with acid (like lemon juice) to reduce harmful compounds formed during high-heat cooking.
Stir-frying quickly cooks ingredients, retaining nutrients and texture. Use minimal oil in a non-stick pan or wok.
Slow cooking tenderizes lean meats and infuses flavors without added fats. It's ideal for making nutrient-rich soups and stews.
Batch cooking helps prepare healthy meals in advance, making it easier to stick to a diabetes-friendly eating plan.
Hydration and Diabetes
Proper hydration is crucial for managing diabetes. The right beverage choices can help maintain blood sugar levels while keeping the body well-hydrated.
Best Drinks for Hydration
Water is the top choice for hydration in diabetes management. It has no calories or carbohydrates, making it ideal for blood sugar control. Low-calorie drinks like unsweetened tea and sparkling water are excellent alternatives. These options provide variety without added sugars.
Herbal teas offer hydration with potential health benefits. Some, like chamomile or peppermint, may have properties that support diabetes management. Coffee, when consumed in moderation and without added sugars, can be part of a balanced hydration plan.
For those who find plain water unappealing, infusing it with cucumber, lemon, or berries can add flavor without calories. This encourages increased fluid intake throughout the day.
Impact of Beverages on Blood Sugar
Sugary drinks can cause rapid spikes in blood glucose levels. Sodas, fruit juices, and sweetened teas should be limited or avoided. Even natural fruit juices can raise blood sugar quickly due to their concentrated sugar content.
Alcohol can have complex effects on blood sugar. It may initially lower levels but can lead to highs later. Moderation is key, and drinking with food is advisable.
Some drinks can have surprising effects. For example, certain vegetable juices may be lower in sugar but still impact blood glucose. Always check labels for carbohydrate content.
Milk provides hydration but also contains natural sugars. Low-fat or skim milk can be incorporated into a diabetes meal plan in moderation.
Navigating Restaurant Meals and Takeout
Managing diabetes while dining out or ordering takeout requires smart choices and adaptations. By selecting the right foods and modifying dishes, people with diabetes can enjoy restaurant meals while maintaining blood sugar control.
Smart Choices When Dining Out
Look for grilled, roasted, or baked options on menus. Branzino with vegetables is an excellent choice at Italian restaurants. Opt for lean proteins like chicken or fish. At salad bars, load up on leafy greens, broccoli, and bell peppers. Choose whole grain options when available.
Avoid fried foods, creamy sauces, and sugary drinks. Ask for dressings and sauces on the side. Request steamed vegetables instead of starchy sides. Consider splitting large portions with a dining companion.
Check menus online before going out. This allows time to plan meals that fit within diabetes management goals. Arrive at restaurants slightly hungry, not famished, to prevent overeating.
How to Adapt Restaurant Meals for Diabetes
Use the diabetes plate method to balance restaurant meals. Fill half the plate with non-starchy vegetables. Add a quarter plate of lean protein and a quarter plate of carbohydrates. Ask for substitutions to achieve this balance if needed.
Request modifications to make dishes diabetes-friendly. Ask for grilled chicken instead of breaded, or vegetables instead of fries. Inquire about low-carb options or smaller portion sizes. Many restaurants are willing to accommodate dietary needs.
Be mindful of portion sizes. Take half the meal home for later if portions are large. Skip the bread basket or limit yourself to one small piece. Choose fruit-based desserts or share a dessert to satisfy cravings without overindulging.