Optimizing Dinner Time for Diabetes Management: Timing, Portions, and Balanced Meals
Dinner time for people with diabetes plays a crucial role in managing blood sugar levels. Choosing the right foods and timing meals appropriately can significantly impact glucose control throughout the evening and overnight. Eating a diabetes-friendly dinner 2-3 hours before bedtime allows blood glucose to stabilize before sleep.
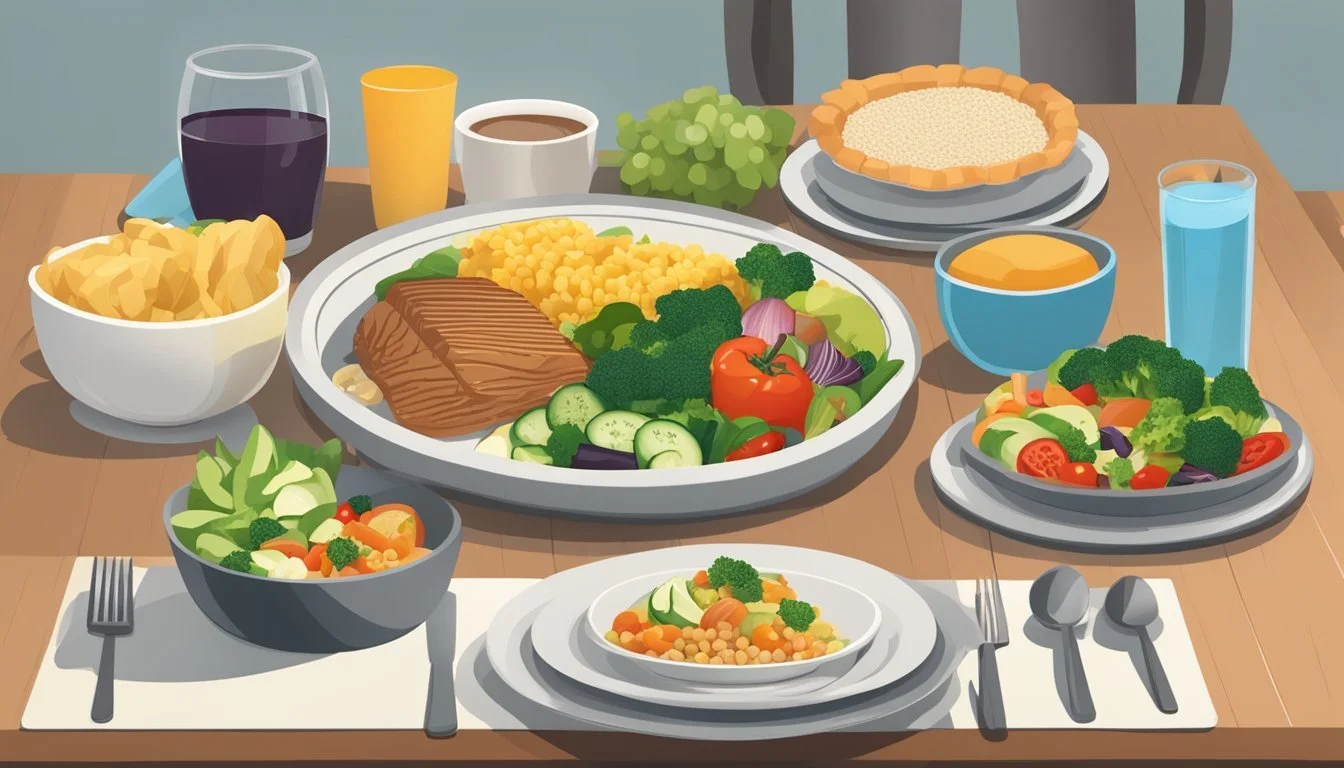
Crafting nutritious and delicious diabetes-friendly dinners doesn't have to be complicated. Many healthy dinner recipes incorporate lean proteins, non-starchy vegetables, and complex carbohydrates to create balanced meals. These components help regulate blood sugar while providing essential nutrients and satisfying flavors.
Incorporating regular exercise into a diabetes management plan can further enhance the benefits of proper meal timing. Research suggests that light physical activity after dinner may help lower blood sugar levels. This combination of mindful eating and movement supports overall diabetes control and promotes better health outcomes.
Understanding Diabetes and Dietary Needs
Diabetes management hinges on balancing food intake with blood sugar levels. Proper meal planning, especially for dinner, plays a crucial role in maintaining stable glucose levels and overall health.
The Impact of Dinner on Blood Sugar Control
Dinner choices significantly affect overnight and morning blood sugar levels. Consuming a balanced meal helps prevent blood sugar spikes and dips. Opt for fiber-rich vegetables, lean proteins, and moderate portions of complex carbohydrates.
A well-planned dinner can stabilize blood sugar for hours after eating. This is particularly important for preventing nighttime hypoglycemia or morning hyperglycemia.
Consider the timing of dinner in relation to bedtime. Eating too late may lead to elevated blood sugar levels during sleep.
Macronutrients and Diabetes Management
Balancing macronutrients is key for effective diabetes management. Carbohydrates have the most direct impact on blood sugar levels.
Carbohydrates: Choose complex carbs like whole grains, legumes, and vegetables. These provide steady energy and essential nutrients.
Protein: Include lean protein sources such as fish, poultry, or plant-based options. Protein helps slow digestion and stabilize blood sugar.
Fats: Incorporate healthy fats from sources like avocados, nuts, and olive oil. They aid in nutrient absorption and promote satiety.
Aim for a balanced plate: 1/4 protein, 1/4 carbohydrates, and 1/2 non-starchy vegetables.
The Importance of Routine in Meal Planning
Establishing a consistent dinner routine supports better blood sugar control. Regular meal times help the body anticipate and regulate glucose levels more effectively.
Create a meal plan that fits your lifestyle and preferences. This makes it easier to stick to healthy eating habits long-term.
Consider using tools like the Diabetes Plate method to simplify meal planning. This approach ensures balanced portions without complex calculations.
Consistency in portion sizes and meal composition aids in predicting insulin needs and maintaining stable blood sugar levels.
Designing a Diabetes-Friendly Dinner
Creating a diabetes-friendly dinner involves balancing nutrients, controlling portions, and selecting foods that help maintain stable blood sugar levels. The key is to focus on nutrient-dense ingredients while limiting refined carbohydrates and unhealthy fats.
Caloric Considerations for Evening Meals
Dinner should provide about 20-30% of daily caloric needs for most people with diabetes. This typically ranges from 400-600 calories, depending on individual requirements. Eating at regular times helps stabilize blood sugar.
Spreading calories evenly throughout the day prevents large spikes in glucose levels. Smaller, more frequent meals can be beneficial for some individuals. Consulting a registered dietitian can help determine optimal calorie distribution.
Choosing the Right Mix of Foods
A diabetes-friendly dinner plate should include a mix of complex carbohydrates, lean proteins, and healthy fats. Aim for 1/4 of the plate to be whole grains or starchy vegetables, 1/4 lean protein, and 1/2 non-starchy vegetables.
Whole grains like quinoa, brown rice, or whole wheat pasta provide fiber and nutrients. Lean proteins such as chicken, fish, tofu, or beans help with satiety. Non-starchy vegetables add volume and nutrients with minimal impact on blood sugar.
Incorporate healthy fats from sources like olive oil, avocado, or nuts in moderation. These fats can help slow digestion and reduce post-meal blood sugar spikes.
Creating Balanced Plates with Low-Carb Options
Low-carb dinners can be an effective strategy for managing blood sugar. Focus on filling the plate with non-starchy vegetables and lean proteins. Examples include:
Grilled salmon with roasted broccoli and cauliflower rice
Chicken stir-fry with mixed vegetables and a small portion of brown rice
Beef and vegetable soup with a side salad
Incorporate low-glycemic index foods like legumes, which provide carbohydrates that are slowly digested. Use herbs and spices to add flavor without extra calories or carbs.
For those who prefer higher-carb options, practice portion control and pair carbs with protein and fiber to slow digestion. Always monitor blood glucose responses to different meal compositions to find what works best.
Nutrient-Rich Ingredients for Diabetes
Selecting the right ingredients is crucial for managing blood sugar levels and maintaining overall health with diabetes. Focusing on nutrient-dense foods provides essential vitamins, minerals, and macronutrients while keeping carbohydrate intake in check.
Protein Choices for Sustained Energy
Lean proteins play a vital role in diabetes management by providing sustained energy without spiking blood sugar. Chicken and turkey breast are excellent low-fat options, offering about 25 grams of protein per 3-ounce serving. Lean beef cuts like sirloin or flank steak can be included in moderation, providing iron and B vitamins.
Fish, especially fatty varieties like salmon, mackerel, and sardines, offer heart-healthy omega-3 fatty acids. Egg whites and low-fat dairy products are also valuable protein sources. Plant-based proteins such as tofu, tempeh, and seitan can be incorporated for variety and additional fiber.
Vegetables and Legumes for Fiber Intake
Non-starchy vegetables are essential for diabetes-friendly meals, providing fiber, vitamins, and minerals with minimal impact on blood sugar. Leafy greens like spinach, kale, and arugula are rich in nutrients and low in calories. Cruciferous vegetables such as broccoli, cauliflower, and Brussels sprouts offer additional health benefits.
Legumes like lentils, chickpeas, and kidney beans provide a powerful combination of protein and fiber. A half-cup serving of cooked lentils contains about 9 grams of protein and 8 grams of fiber. Quinoa, a versatile pseudo-grain, offers complete protein and fiber, making it an excellent choice for diabetes management.
Healthy Fats and Their Role
Incorporating healthy fats into meals helps slow digestion and stabilize blood sugar levels. Avocados are rich in monounsaturated fats and provide about 10 grams of fiber per medium fruit. Nuts and seeds, such as almonds, walnuts, and chia seeds, offer a mix of healthy fats, protein, and fiber.
Olive oil is an excellent source of monounsaturated fats and can be used for cooking or as a salad dressing. Fatty fish like salmon provide omega-3 fatty acids, which may help reduce inflammation and improve insulin sensitivity. Including these healthy fat sources in moderation can enhance meal satisfaction and nutrient absorption.
Diabetes-Friendly Dinner Recipes
Nutritious and delicious dinner options can help manage blood sugar levels while satisfying hunger. These recipes focus on lean proteins, complex carbohydrates, and plenty of vegetables to create balanced meals for those with diabetes.
Meat-Based Diabetes-Friendly Dishes
Lean meats provide protein without excess saturated fat. Balsamic-glazed beef skewers offer a flavorful option, pairing well with brown rice and a tossed salad. For a comforting meal, try turkey meatballs with whole wheat pasta and a side of roasted vegetables.
Pork tenderloin is another excellent choice. Marinate it in herbs and lemon juice, then grill or roast alongside colorful bell peppers and onions. Chicken remains a versatile staple - try it grilled with a quinoa and vegetable salad or baked with a crispy almond coating.
For seafood lovers, charred shrimp with pesto over quinoa provides a nutrient-dense meal. Pair it with steamed broccoli for added fiber and vitamins.
Plant-Based Meals for Overall Health
Vegetarian options can be both diabetes-friendly and satisfying. Zucchini lasagna replaces pasta with thin slices of zucchini, layered with low-fat ricotta and marinara sauce. This dish reduces carbs while maintaining flavor.
Curry dishes packed with vegetables and chickpeas offer a warming, spice-filled meal. Serve over cauliflower rice to keep carbohydrates in check. Bean-based chili provides fiber and protein, helping to stabilize blood sugar levels.
For a twist on pizza night, try a cauliflower crust topped with plenty of vegetables and a moderate amount of low-fat cheese. This satisfies cravings while keeping carb intake manageable.
Quick and Easy Diabetes Dinners
Sheet-pan meals simplify cooking and cleanup. Try chicken and vegetables seasoned with rosemary, roasted together for a complete meal in under 30 minutes. Beef and bean sloppy joes offer a healthier take on the classic, ready in just half an hour.
One-pot dishes like garlicky shrimp and spinach come together quickly and minimize dishes. Pair with a small portion of whole grain pasta or brown rice. For a meatless option, whip up a vegetable and tofu stir-fry with a low-sodium sauce.
Salad bowls with grilled chicken or fish, mixed greens, and a variety of colorful vegetables make for a refreshing and easy dinner. Add a small amount of quinoa or farro for complex carbohydrates.
Meal Timing and Blood Sugar Stabilization
Meal timing plays a crucial role in managing blood sugar levels for people with diabetes. Strategic scheduling of meals and snacks can help stabilize glucose throughout the day and night.
The Best Time to Have Dinner
Eating dinner earlier in the evening can benefit blood sugar control. Aim to finish your last meal 2-3 hours before bedtime. This allows time for digestion and helps prevent nighttime blood sugar spikes.
A study suggests that having a larger breakfast and smaller dinner may improve glucose levels and decrease insulin requirements. Consider shifting more calories to earlier in the day if possible.
For those who exercise in the evening, timing dinner shortly after physical activity can help replenish energy stores and stabilize blood sugar. Pair carbohydrates with protein and healthy fats to slow digestion and glucose absorption.
Snacks and Post-Dinner Eating Habits
Avoiding late-night snacking is generally recommended for better glucose management. If needed, opt for a small snack of 15 grams of carbs with some protein before bed.
Good options include:
A small apple with peanut butter
Greek yogurt with berries
A handful of nuts and a few whole-grain crackers
These choices provide steady energy without causing dramatic blood sugar fluctuations overnight. Be mindful of portion sizes to prevent excess calorie intake.
Exercise and Meal Timing Synergy
Coordinating exercise with meal timing can enhance blood sugar control. Engaging in physical activity like cycling or brisk walking after meals can help lower post-meal glucose spikes.
Try to incorporate movement into your daily routine:
Take a 15-minute walk after dinner
Do some light stretching or yoga in the evening
Perform resistance exercises before meals to improve insulin sensitivity
For longer or more intense workouts, eat a balanced meal 1-2 hours before exercising. This provides fuel for the activity while avoiding digestive discomfort.
Remember to monitor blood sugar levels before, during, and after exercise to understand how your body responds to different timing strategies.
Lifestyle Considerations for Diabetes Management
Managing diabetes effectively involves adopting a comprehensive approach to daily habits and choices. Key lifestyle factors can significantly impact blood sugar control and overall health outcomes for individuals with diabetes.
Weight Loss Strategies and Dietary Adjustments
Weight management plays a crucial role in diabetes control. Losing excess weight can improve insulin sensitivity and blood sugar levels. A balanced diet focusing on portion control and nutrient-dense foods is essential.
Opt for high-fiber vegetables, lean proteins, and whole grains. These foods help stabilize blood sugar and promote satiety. Limit processed foods, sugary drinks, and excessive carbohydrates.
Meal planning and tracking food intake can aid weight loss efforts. Consider using a food diary or smartphone app to monitor calorie intake and nutritional balance.
Physical Activity's Role in Diabetes Management
Regular exercise is a cornerstone of diabetes management. Physical activity helps lower blood sugar levels and improves insulin sensitivity. Aim for at least 150 minutes of moderate-intensity aerobic activity per week.
Incorporate a mix of cardiovascular exercises and strength training. Walking, swimming, and cycling are excellent low-impact options. Resistance exercises help build muscle mass, which can improve glucose metabolism.
Always check blood sugar levels before, during, and after exercise. Adjust insulin or medication as needed, and keep fast-acting carbohydrates on hand to prevent hypoglycemia.
Avoiding Complications Through Nutritional Choices
Proper nutrition is key to preventing diabetes-related complications. Focus on heart-healthy foods to reduce the risk of cardiovascular disease, a common concern for people with diabetes.
Choose foods rich in omega-3 fatty acids, such as fatty fish, nuts, and seeds. These can help lower inflammation and protect heart health.
Limit sodium intake to manage blood pressure. Opt for fresh herbs and spices instead of salt to flavor meals.
Maintain adequate vitamin and mineral intake through a varied diet or supplements as recommended by a healthcare provider. This can support overall health and potentially reduce the risk of diabetes-related complications.