The Ultimate Guide to Organizing Your Kitchen for a Low-FODMAP Diet
Streamlining Your Space for Healthful Living
Embarking on a low-FODMAP diet can be transformative for individuals managing irritable bowel syndrome (IBS). The diet, which involves limiting foods high in certain fermentable carbohydrates, is endorsed by dietitians as a strategic approach to identify triggers and reduce IBS symptoms. Organizing the kitchen to support this dietary plan is crucial for success, as it simplifies meal preparation and helps in adhering to the diet's guidelines.
With the array of foods and ingredients typically found in a kitchen, transitioning to a low-FODMAP diet requires a clear understanding of which items are compliant and how to store them effectively. This ensures that individuals can effortlessly access and combine low-FODMAP foods to create enjoyable and symptom-free meals. Establishing sections for low-FODMAP ingredients and preparing meals ahead of time are some of the strategies that can assist in maintaining this dietary regimen.
Understanding FODMAPs
In managing symptoms related to various digestive disorders, the science behind FODMAPs plays a critical role, as does the identification of high-FODMAP foods and the potential health benefits of a low-FODMAP diet.
Science of FODMAPs and Digestion
FODMAPs stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. These short-chain carbohydrates are not fully absorbed by the gut and can be fermented by bacteria in the intestine. The fermentation process can cause excessive water to be drawn into the gut, leading to symptoms such as bloating, gas, and abdominal pain. Research indicates that a diet low in FODMAPs can alleviate these symptoms for many individuals with sensitivity to these carbohydrates.
Identifying High-FODMAP Foods
High-FODMAP foods include a variety of fruits, vegetables, grains, and dairy products. Key examples include:
Fruits: apples, cherries, pears
Dairy: milk, yogurt, ice cream
Sweeteners: high-fructose corn syrup, honey
It's crucial for individuals to recognize that foods containing fructose in excess of glucose and food products with added polyols like sorbitol and mannitol are high in FODMAPs. Similarly, dairy products high in lactose also fall into this category.
Health Benefits of a Low-FODMAP Diet
Adopting a low-FODMAP diet can have notable health benefits, particularly for individuals with irritable bowel syndrome (IBS) or similar gastrointestinal disorders. By reducing intake of foods high in FODMAPs, one may experience less digestive distress, decreased inflammation within the gut, and an overall improvement in quality of life. It is, however, important that such dietary changes are made under professional guidance to ensure nutritional adequacy.
Starting the Low-FODMAP Diet
Initiating a low-FODMAP diet involves a structured approach that includes an elimination phase followed by a reintroduction phase, aiming for a long-term solution to manage symptoms effectively.
The Elimination Phase
The elimination diet is the first step, designed to identify triggers by removing high-FODMAP foods from one's diet and replacing them with low-FODMAP alternatives. This phase typically spans from 2 to 6 weeks. An individual may begin to notice symptom relief within a few days, but for some, it might take a few weeks to observe changes.
Reintroduction Phase
Once an individual sees improvement in symptoms during the elimination phase, they enter the reintroduction phase. This involves carefully reintroducing one high-FODMAP food at a time back into the diet over a three-day period to monitor for any symptom recurrence. Detailed tracking of the body's responses helps identify specific triggers.
Creating a Long-Term Solution
The goal is to establish a diet that is less restrictive but still successful in managing symptoms. The individual learns to balance low-FODMAP choices with limited quantities of high-FODMAP foods that they can tolerate, striving toward a personalized, sustainable eating plan. This individualized approach helps ensure nutritional adequacy while keeping symptoms at bay.
By methodically following these phases, the likelihood of long-term success increases, and the individual can enjoy a wider variety of foods without undue discomfort.
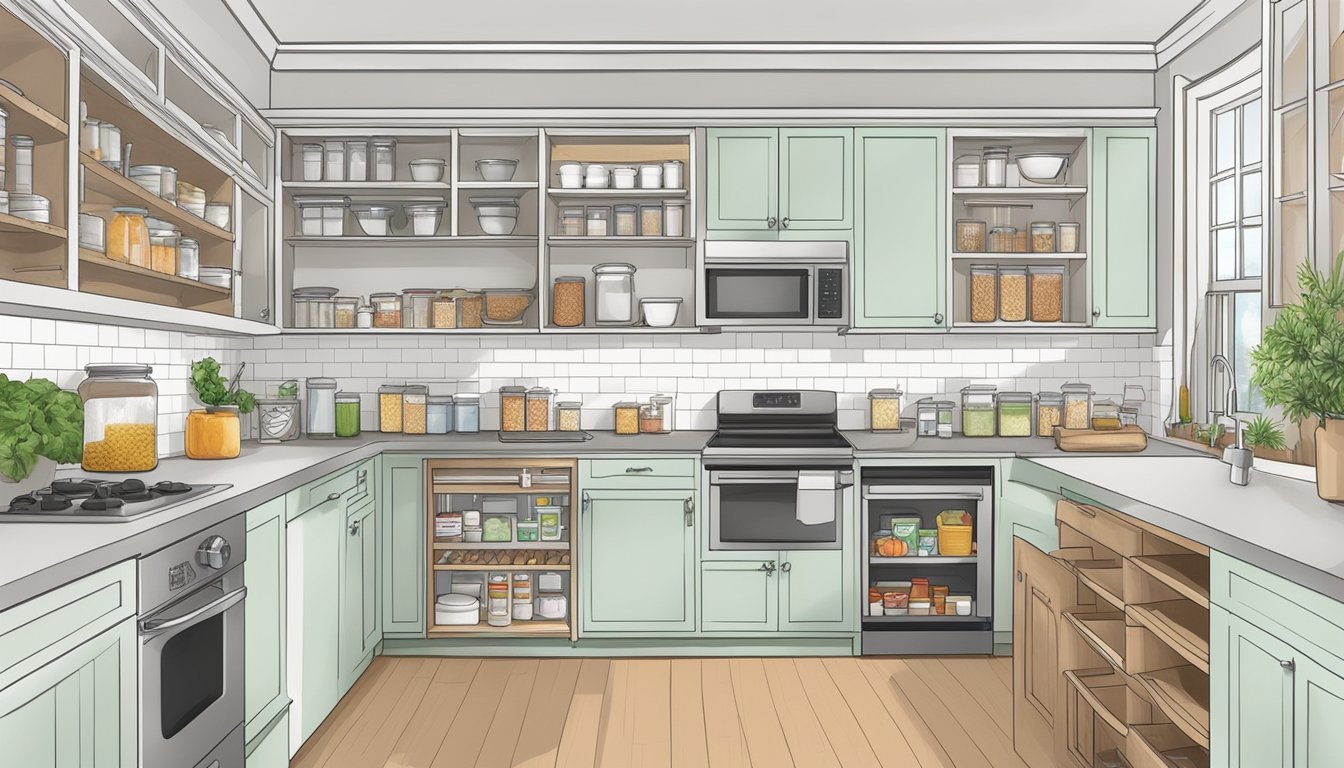
Low-FODMAP Kitchen Organization
Organizing a kitchen to accommodate a Low-FODMAP diet involves identifying essential staples, implementing smart storage solutions, and diligent labeling to prevent cross-contamination. These strategies facilitate ease of meal preparation and can significantly reduce symptoms for individuals sensitive to high-FODMAP foods.
Essential Low-FODMAP Staples
A well-organized Low-FODMAP kitchen starts with stocking the right ingredients. One should include a variety of:
Grains: Rice, oats, and quinoa.
Proteins: Eggs, firm tofu, and unseasoned meats.
Dairy alternatives: Lactose-free milk, almond milk, and hard cheeses.
Condiments: Garlic-infused oils, pure maple syrup, and soy sauce alternatives like tamari (gluten-free).
Vegetables and Fruits: Bell peppers, carrots, bananas, and oranges.
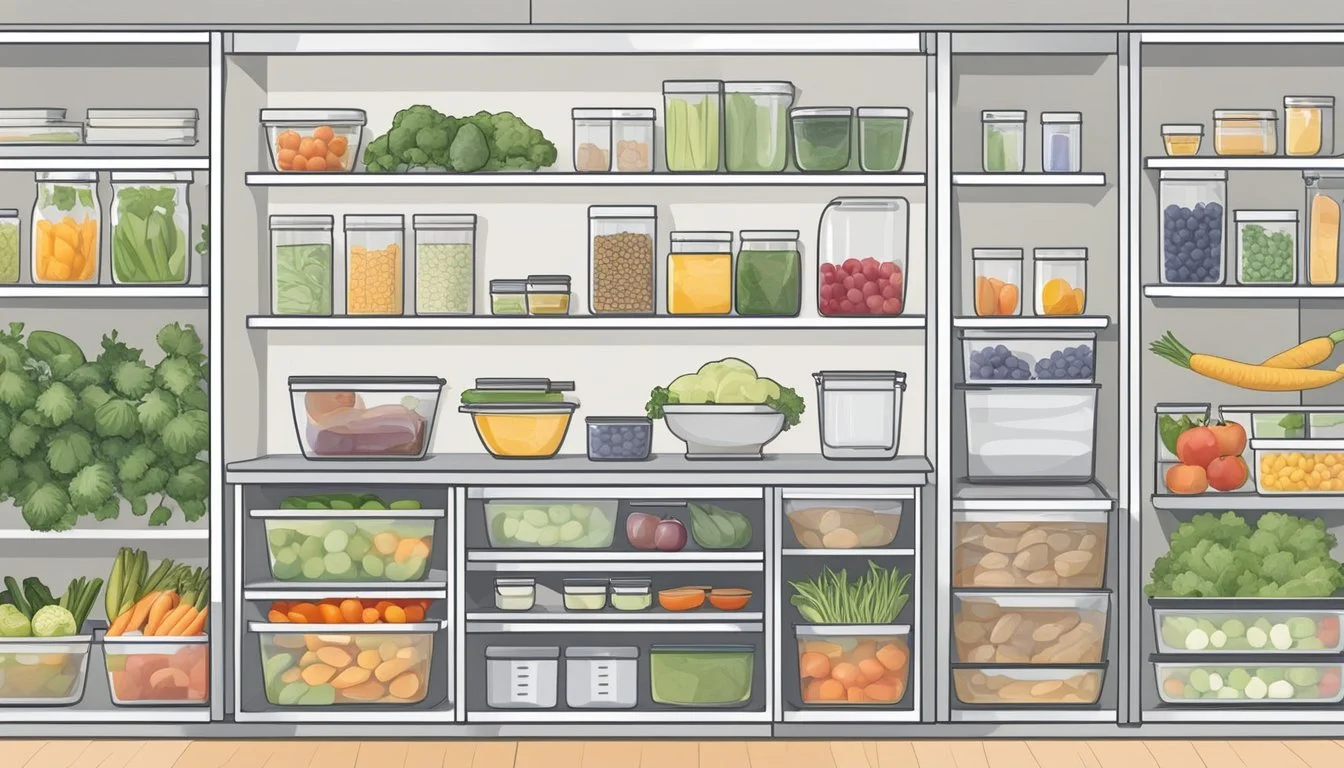
Create a dedicated space in your pantry and refrigerator for these Low-FODMAP staples to ensure they are easily accessible.
Low-FODMAP Storage Tips
Effective storage is key to maintaining the freshness and integrity of Low-FODMAP foods:
Refrigeration: Keep dairy alternatives and perishable proteins in the coldest part of the refrigerator to extend shelf life.
Airtight Containers: Store grains and nuts in clear, airtight containers to protect against moisture and pests.
Separation: Allocate separate shelves or bins for Low-FODMAP foods to minimize the risk of accidentally using high-FODMAP ingredients.
Using clear containers not only helps in identifying food items quickly but also in monitoring quantities for timely restocking.
Labeling and Avoiding Cross-Contamination
Cross-contamination can easily occur in a busy kitchen, but it is preventable with these steps:
Clear Labeling: Use labels to mark containers with 'Low-FODMAP' or the name of the contents. For multi-ingredient meals, include preparation dates.
Utensils and Cookware: Designate specific utensils and cutting boards for Low-FODMAP foods. Consider color-coding to avoid mix-ups.
Gluten-Free Consideration: If gluten is a concern, ensure all surfaces, utensils, and cookware are thoroughly cleaned before preparing gluten-free Low-FODMAP meals.
Good organization reduces risks, streamlining the cooking process and ensuring compliance with dietary needs.
Navigating Common Challenges
When adopting a low-FODMAP diet, individuals often face hurdles such as finding appropriate ingredient substitutes, managing additional food sensitivities, and maintaining their diet in social settings. Here's how one can skilfully address these common challenges.
Substituting High-FODMAP Ingredients
Onions and garlic are high in FODMAPs and commonly used flavor enhancers that require effective substitutes. One might use garlic-infused oil or asafoetida powder to replicate the flavor without introducing FODMAPs. Alternative ingredients should be checked against the Monash FODMAP app to ensure they are safe to consume.
Bread: Options made from wheat are high in FODMAPs; alternatives like spelt sourdough or gluten-free bread can be used instead.
Pasta: One can opt for rice, quinoa, or gluten-free pasta that don't contain high FODMAP grains.
Milk: Lactose-free dairy or plant-based milks like almond or rice milk serve as viable replacements.
Ensuring a kitchen stocked with low-FODMAP substitutes prevents accidental consumption of high-FODMAP ingredients.
Dealing with Food Sensitivities and Allergies
Individuals may have sensitivities or allergies in addition to FODMAP restrictions. It’s important to tailor the diet to accommodate both low-FODMAP guidelines and any additional dietary requirements. For instance, if someone has a gluten allergy on top of FODMAP sensitivity, they should source gluten-free alternatives that also comply with low-FODMAP standards.
Careful label reading is crucial to avoid hidden allergens and FODMAPs.
Using the Monash FODMAP app can aid in identifying products that cater to both FODMAP constraints and additional allergies.
Eating Out and Social Situations
Eating out or attending social events poses significant challenges, as one often encounters high-FODMAP foods. She can manage these scenarios by:
Reviewing the menu in advance and identifying potential dishes that meet low-FODMAP criteria.
Communicating dietary restrictions clearly to the staff to ensure meals are prepared with appropriate modifications.
Carrying low-FODMAP snacks in case suitable food options are not available.
By preparing in advance and steering clear of high-FODMAP offerings, she can stick to her dietary plan even when outside her own kitchen.
FODMAP-Friendly Cooking and Recipes
Navigating a low-FODMAP diet requires thoughtful meal planning and preparation, as well as familiarity with ingredient substitutions. This section offers practical advice on organizing your kitchen to create satisfying meals that adhere to FODMAP guidelines.
Meal Planning and Prepping
Meal planning for a low-FODMAP diet is essential to reduce symptoms and maintain a nutritious diet. Individuals should start by creating a weekly menu that incorporates a variety of FODMAP-friendly foods. They might consider preparing larger batches of safe vegetables and proteins, such as chicken or tempeh (What wine goes well with tempeh?), ahead of time to streamline cooking throughout the week. Maintaining a well-organized pantry with low-FODMAP staples such as rice, gluten-free pasta, and pure spices can simplify meal preparation. Pre-washed and chopped vegetables stored in the refrigerator are convenient for quick meal assembly.
Low-FODMAP Recipes and Ideas
Numerous recipes fit within low-FODMAP guidelines while still providing flavorful and satisfying meals. Here are a few recipe ideas:
Proteins: Marinated tofu or tempeh can provide a protein-rich basis for many dishes, such as stir-fries without garlic or onions.
Breakfast: Scrambled eggs with permitted vegetables like bell peppers and spinach can provide a hearty start to the day.
Pasta: A roasted red pepper pasta using gluten-free noodles and a sauce made from allowed ingredients offers comfort without the FODMAPs.
When cooking, individuals should use simple methods like grilling, baking, or sautéing with safe oils, and always be mindful of serving sizes for higher FODMAP ingredients that are safe in smaller amounts.
Adjusting Serving Sizes for Tolerance
The tolerance for FODMAPs can vary greatly among individuals, so serving sizes should be adjusted accordingly. For example, while eggs are low in FODMAPs and can be eaten more freely, other ingredients such as tofu have recommended serving size limits. It's useful for individuals to keep a food diary to track their tolerance levels and identify which foods and serving sizes do not trigger symptoms. Smaller, more frequent meals often aid in digestion and help manage FODMAP intake throughout the day.
Managing Symptoms with a Low-FODMAP Diet
Embarking on a Low-FODMAP Diet is a strategic way to alleviate digestive discomforts such as bloating, gas, constipation, and diarrhea. This section outlines methods to track symptoms in relation to food intake, discusses the value of a dietitian's expertise, and indicates when it's appropriate to consult a doctor for medical advice.
Tracking Symptoms and Food Intake
Tracking one's food intake and any subsequent symptoms is crucial for identifying which foods exacerbate digestive issues. It’s advisable for individuals to maintain a detailed food diary that juxtaposes what they eat with the digestive symptoms they experience. For clarity, they should note:
Dates and times of meals
Portion sizes
Ingredients of each meal
Symptoms experienced
Severity of symptoms, on a scale of 1-10
Duration of symptoms after eating
This diary will serve as a comprehensive log to help discern patterns over time.
The Role of Dietitian in Symptom Management
A registered dietitian plays an instrumental role in tailoring a Low-FODMAP Diet to an individual’s specific needs. They can provide:
Personalized meal planning that systematically eliminates high FODMAP foods
Guidance on appropriate serving sizes
Advice on nutrient-rich, low FODMAP alternatives
Support during the reintroduction phase to identify food intolerances
Strategies for maintaining a balanced diet
Consulting a dietitian ensures a methodical approach to the diet and helps avoid nutritional deficiencies.
When to Seek Medical Advice
While a Low-FODMAP Diet can be managed with the help of a dietitian, consulting a doctor is essential if symptoms persist or worsen. One should seek medical advice if they experience:
Significant changes in the frequency or nature of symptoms
Severe or acute pain that is not managed by diet alone
Any concerning symptoms, such as unintentional weight loss or blood in the stool
A doctor may perform additional tests or adjust treatment plans to ensure the best care for one's specific health needs.
Beyond the Diet: Lifestyle Considerations
In managing a low-FODMAP diet, it's equally important to recognize the relationship between lifestyle habits and their impact on irritable bowel syndrome (IBS). Addressing stress, incorporating regular physical activity, and ensuring a balanced diet are crucial for gut health and overall well-being.
Stress Management and IBS
Individuals with IBS often find that their symptoms are closely linked to stress levels. Effective stress management techniques include mindfulness meditation, regular exercise, and adequate sleep. Techniques such as deep breathing exercises and yoga can also help to reduce the stress that may exacerbate gastrointestinal symptoms.
Physical Activity and Gut Health
Physical activity is well-documented to support healthy digestive function. Engaging in moderate exercise for at least 150 minutes per week is recommended and can include activities such as brisk walking, swimming, or cycling. This not only helps in maintaining a healthy weight but also improves gut motility and can relieve stress.
Maintaining a Balanced Diet and Nutrition
While following a low-FODMAP diet, it's essential to maintain overall nutritional balance. One should aim to include:
A variety of low-FODMAP vegetables and fruits to ensure an adequate intake of vitamins and minerals.
Sufficient lean protein sources, such as chicken, fish, eggs, and certain plant-based options like tempeh.
Whole grains like quinoa and gluten-free bread that are low in FODMAPs but high in fiber for maintaining digestive regularity.
It's imperative to ensure that the pursuit of a low-FODMAP lifestyle does not lead to nutritional deficiencies. Consulting a healthcare provider or a registered dietitian can provide personalized guidance to achieve nutritional adequacy while adhering to the dietary restrictions.
Supplements and Medication
When undertaking a low-FODMAP diet, one must pay careful attention to the supplements and medications they incorporate into their routine, as these can impact digestion and symptoms related to functional gastrointestinal disorders.
Probiotics and Gut Bacteria
Probiotics are live microorganisms that can provide health benefits when consumed by maintaining or restoring the gut flora. For individuals on a low-FODMAP diet, probiotics can be particularly helpful in managing gut bacteria and improving digestive health. However, it is crucial to select probiotic supplements that do not contain high-FODMAP ingredients such as lactose or fructooligosaccharides.
Medications for Symptom Control
Many individuals find that medications are necessary to manage specific symptoms of gastrointestinal discomfort. When organizing a kitchen, one should ensure that their medication for symptom control adheres to their dietary needs. Some medications may contain inactive ingredients like lactose or sorbitol, which are high in FODMAPs and can trigger symptoms.
Understanding the Role of Supplements
Supplements can play a significant role in providing essential nutrients that might be missed due to the dietary restrictions of the low-FODMAP diet. When incorporating supplements, it is crucial to choose those free from high-FODMAP excipients such as inulin, which is often used as a filler. Individuals should also check for common high-FODMAP ingredients like wheat-based products or sweeteners such as honey and agave syrup that could exacerbate their symptoms. Consulting with a healthcare provider or a dietitian can guide choosing the right supplements while following a low-FODMAP diet.
Conclusion
Adopting a low-FODMAP diet can be a substantial step for individuals dealing with gastrointestinal conditions. Symptom control is critical, and identifying trigger foods is a fundamental aspect of managing one's well-being. Organizing the kitchen effectively becomes a pivotal task to ensure the path to relief is as smooth as possible.
It is advised that one maintains a well-structured environment where low-FODMAP options are readily accessible. This organization limits the accidental intake of high-FODMAP foods that may lead to symptom flare-ups. Labeling shelves or using separate storage containers can serve as a visual guide to safe food choices.
A few accessible low-FODMAP items one might include are:
Proteins such as eggs and meats
Lactose-free dairy products
Gluten-free grains like rice and oats
Fruits such as oranges and strawberries
Vegetables like carrots and cucumbers
However, what works for one person might not suit another. Personalization is key, and one must be willing to adapt their kitchen setup as they proceed with the diet and learn more about their personal triggers. This process of adjustment is a normal and necessary part of the low-FODMAP journey.
Tracking symptoms and reactions to reintroduced foods is highly beneficial. It assists individuals in determining which foods they can reincorporate and in what quantities. By doing so, one can enjoy a variety of foods while keeping their symptoms in check.
Persistence and patience are virtues here. Over time, individuals often find a suitable balance that offers symptom relief without imposing too many dietary restrictions, allowing them to enjoy a diverse, flavorful, and nutritious diet.